The authors report an original case using cerebral retrograde perfusion alternating with carotid artery anterograde perfusion, during the surgical treatment of acute ascending aorta dissection. The patient was discharged on 32nd post-operative day in a clinically controlled condition. The Mini Mental State Examination test was applied after 30 days and showed normal cerebral cognitive activity. The authors believe that this method can give a protective effect to the brain during procedures involving aortic dissection or aneurysms, after evaluating its use after a significant series of cases.
Os autores relatam o uso de perfusão cerebral retrógrada e anterógrada para proteção cerebral, em normotermia, durante tratamento cirúrgico de dissecção aguda de aorta do Tipo 1. O paciente foi considerado neurologicamente apto ao ser submetido ao Mini Mental State Examination, no pós-operatório tardio. Os autores acreditam que a associação dos métodos possa se constituir em uma alternativa para proteção cerebral nas operações para tratamento dos aneurismas e dissecções da aorta, após avaliação de seu emprego em uma série significante de pacientes.
INTRODUCTION
Although total circulatory arrest and deep hypothermia utilized in the treatment of aneurysms and aortic dissections give better results, these techniques do not totally eliminate the occurrence of neurological injury [1]. Other methods of cerebral perfusion have demonstrated good results in surgeries of aortic diseases [2,3]. The objective of this report is to inform about the alternate use of retrograde and anterograde cerebral perfusion at normothermia, as a method of cerebral protection in the surgical treatment of acute aortic dissection and the results of the late neurological evaluation.
CASE REPORT
A 46-year-old male patient with characteristics of Marfan's Syndrome was attended in the Hospital Emergency Department with acute aortic dissection. The disease was associated to acute myocardial infarction, acute aortic insufficiency, acute renal insufficiency, long-term symptoms and cardiogenic shock.
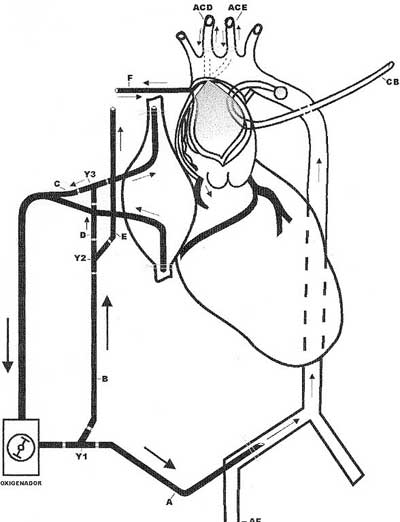
An urgent surgery was performed. The operation was conducted in the routine manner with normothermic cardiopulmonary bypass (CPB), which was established and utilized according to Figure 1.
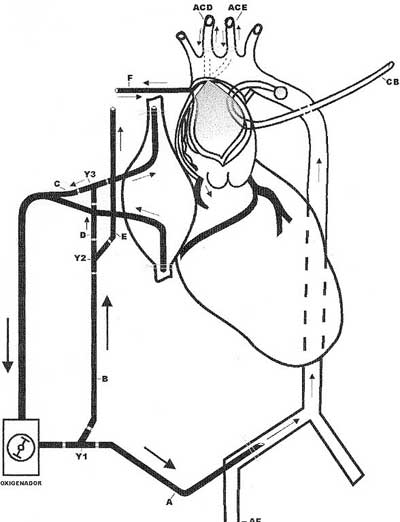
Fig. 1 - Schematic design of the cardiopulmonary bypass system used. Line A (femoral perfusion); Line B (retrograde D-perfusion, anterograde E-perfusion); Line C (normal venous drainage of the vena cavas); Line F (perfusion of the carotid arteries). CB - balloon catheter; Y1, Y2, Y3 - Y-shaped connectors; ACD - right carotid artery; ACE - left carotid artery; AF - femoral artery
Subsequently at normothermia, a number 32 valved tubular prosthesis with a number 27 St. Jude prosthesis were implanted, as the annulo-aortic ectasia was great and there was significant aortic insufficiency due to dilation of the valve annulus and collapse of the non-coronary cusp.
Infusion of cold crystalloid cardioplegic solution was made at twenty-minute intervals to the ostia of the coronary arteries. The left coronary artery ostium was implanted in the tubular prosthesis, utilizing a continuous 6-0 prolene suture. An autogenic saphenous vein bridge was performed to the right coronary artery which was proximally ligated.
At normothermia CPB was interrupted. Retrograde cerebral perfusion was made using Line D, with a flow that varied between (300-500 mL/min.) and the drainage through Line C was interrupted. The ascending aorta was opened lengthwise as far as the pericardial reflection, it was inspected and the right and left coronary arteries were located. Both carotids were cannulated and isolated using external tourniquets. The return flow of the retrograde perfusion was utilized to fill the perfusion cannulae of the carotids (Line F) which, after being filled of blood, were clamped, the air was removed and they were connected to the anterograde perfusion line (Line E), obtained with a 'Y2' connector.
The anterograde flow at 11 mL/kg of body weight/min and interruption of the retrograde perfusion (Line D) were maintained.
The distal approach of the aortic dissection consisted in end-to-end anastomosis to the aorta with a tubular prosthesis. Subsequently, filling of the arterial vascular bed was achieved through femoral arterial cannulization (Line A). Gradually, the anterograde perfusion (Line F) was interrupted and the retrograde perfusion (Line D) was restarted during approximately ten minutes, until the vascular bed was totally filled and the air was removed from the cardiac cavities through the apex of the left ventricle. Normal perfusion through the femoral artery was established and the retrograde cerebral perfusion (Line D) was interrupted. The cardiopulmonary bypass was removed after reaching adequate conditions. The routine procedures followed including the closing of the thorax.
The renal insufficiency was reverted and vasoactive drugs were removed and on the 32nd of hospitalization the patient left the ICU and was discharged from hospital on the 36th postoperative day in a good clinical state. In the late postoperative period the patient was submitted to clinical and cognitive evaluations using the Mini Mental State Examination [4] when a score of 30 was obtained, demonstrating good cognitive activity. A computed tomography of the brain, requested in the late postoperative period was within the normal parameters.
COMMENTS
Cerebral injury influences the results of surgeries of aneurysms and aortic dissections. Evidence of this complication can be best demonstrated by neuropsychological tests [5]. Retrograde cerebral perfusion as proposed by Ueda et al. [2] in 1988, although initially giving excellent results and was reproduced by other authors, with time it was observed that this procedure does not offer total cerebral protection [4]. In 1986, Frist et al. [3] utilizing anterograde cerebral perfusion and moderate hypothermia did not evidence neurological complications in a small series of eight patients submitted to surgery. Possible psychiatric and cognitive disorders in the postoperative period were investigated, which are generally not recognized by surgeons or even by neurologists [6].
Our patient was evaluated using the Mini Mental State Examination [4] a test that is capable of associating cognitive disorders with neurologic disorders. In the test, different degrees of orientation, memory, attention, calculation and language can be assessed using a scoring system of up to 30 points. A score of 23 or less demonstrates a cognitive disorder which can be related to cerebral injury and can be confirmed using cerebral tomography [6]. The use of Mini Mental State Examination has been validated to recognize postoperative alterations as cognitive defects that are related to cortical alterations such as bleeding and transitory ischemic events, as well as subcortical alterations of the central nervous system [6]. Our patient had a score 30.
To confirm that the results of the procedure utilized in this case is a constant reality, it is necessary to reproduce this method in a series of patients.
ACKNOWLEDGEMENTS
The authors with to thank Mrs Adriana Fontes & Mr Luis Gustavo Hilário for their help with the illustration.
BIBLIOGRAPHIC REFERENCES
1. Crawford ES. Progress in treatment of thoracic aortic aneurysms. World J Surg. 1988;12(6):805-9.
2. Ueda Y, Miki S, Kusuhara K, Okita Y, Tahata T, Jinno K et al. Surgical treatment of the aneurysm or dissection involving ascending aorta and aortic arch using circulatory arrest and retrograde perfusion. Nippon Kyobu Geka Gakkai Zasshi.1988;36(2):161-6.
3. Frist WH, Baldwin JC, Starnes VA, Stinson EB, Oyer PE, Miller DC et al. A reconsideration of cerebral perfusion in aortic arch replacement. Ann Thorac Surg. 1986;42(3):273-81.
4. Dick JP, Guiloff RJ, Stewart A, Blackstock J, Bielawska C, Paul EA et al. Mini-mental state examination in neurological patients. J Neurol Neurosurg Psychiatry. 1984;47(5):496-9.
5. Fontes RD, Stolf NAG, Mady C, Ávila LF, D'Élia RS, Parras C et al. Perfusão cerebral retrógrada é método eficaz de proteção cerebral? Resultados imediatos de estudo consecutivo e randomizado. Rev Bras Cir Cardiovasc. 1999;14(1):1-5.
6. Tsai L, Tsuang MT. The mini-mental state test and computerized tomography. Am J Psychiatry. 1979;136(4A):436-8.
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license