Objective: To present the experience of 157 implantations using a simplified technique for coronary sinus catheterization, based on the atrial component of the intracavitary electrogram and radiological anatomy, showing the success rate and total time of radioscopy use.
Method: From October 2001 to February 2005, 157 biventricular pacemaker implantations were performed in previously selected patients, using radiological anatomy and observation of the intracavitary electrogram, focusing on the atrial component. Here we show the success rate, complications and total time of radioscopy use.
Results: The implantation of the system employing left ventricular pacing via the coronary sinus was not possible in 11 patients. Difficulties in cannulation of the coronary ostium were felt in 20 patients and difficulties of lead advancement through the coronary sinus existed in 39 patients. The mean time of radioscopy use was 18.27 ± 15.46 minutes.
Conclusion: The implantation technique, proposed by the author, using the atrial component morphology of the intracavitary electrogram and radiological anatomy proved to be safe and effective for the cannulation of the coronary sinus ostium requiring shorter radioscopy times.
Objetivo: Apresentar a experiência de 157 implantes utilizando uma técnica simplificada para cateterização do seio coronariano, baseada no eletrograma intracavitário e anatomia radiológica, demonstrando o porcentual de sucesso e tempo total de utilização de radioscopia.
Método: De outubro de 2001 a fevereiro de 2005, foram realizados 157 implantes de marcapasso biventricular em pacientes previamente selecionados, utilizando-se anatomia radiológica e observação de eletrograma intracavitário, demonstrando a taxa de sucesso, complicações e tempo total de utilização de radioscopia.
Resultados: O implante do sistema, utilizando-se a estimulação do ventrículo esquerdo via seio coronariano, não foi possível em onze procedimentos. Em 20 pacientes foram observadas dificuldades na canulação do óstio coronário e em 39 pacientes observou-se dificuldade de progressão do eletrodo através do seio coronário. O tempo médio de utilização de radioscopia foi 18,27 ± 15,46 min.
Conclusão: A técnica de implante, proposta pelo autor, utilizando o eletrograma intracavitário e anatomia radiológica, demonstrou ser segura e eficaz para canulação do óstio do seio coronário, necessitando de reduzidos tempos de radioscopia.
INTRODUCTION
Recent studies have demonstrated that cardiac resynchronization through biventricular pacing is a important coadjuvant treatment in optimized medicinal therapy of patients with refractory congestive heart failure caused by chronic left ventricular dysfunction and intraventricular conduction disorders, promoting an improvement in the heart function and the quality of life [1-3].
The technique of left ventricular pacing can be performed both epimyocardially by thoracotomy, or through the epicardium using the transvenous method. Although the latter technique is the gold standard, the greatest limitation of this treatment is the catheterization and insertion of a lead in the coronary sinus (CS) and its branches for left ventricle pacing [4].
The implantation of a specific electrode for left ventricular pacing is a relatively complex procedure, which involves variations in the anatomy of coronary veins, the quality of the material utilized and the surgeon's experience [5]. The impossibility of CS catheterization, variations in the anatomy of coronary venous system and diaphragmatic pacing are the most common reasons for lead placement to be unsuccessful. Failure rates tend to decrease with the development of new electrodes and the surgeon's experience [6-9].
With the good results presented by this coadjuvant treatment, cardiac resynchronization therapy is becoming a routine treatment for pre-selected patients. Due to the complexity of the procedure, the medical-scientific engineering professionals have been investing in the adaptation of materials to facilitate the implantation technique [7,10,11].
The objective of this work is to present four years of experience, based on 157 procedures performed on pre-selected patients submitted to cardiac resynchronization therapy, utilizing a simplified technique of coronary sinus catheterization using the radiological anatomy and intracavitary electrography, demonstrating the success rate, complications and the total time of the utilization of radioscopy.
METHOD
Study Characterization
This study was performed in the Clinical and Cardiovascular Surgery Service "Prof. Dr. Sérgio Almeida de Oliveira" of the Hospital Real and Benemérita Sociedade Portuguesa de Beneficência de São Paulo. The data collected were of patients submitted to biventricular pacemaker implantation from October 2001 to February 2005. The study was divided into three phases of observation for the evaluation of the success rate and time of utilization of radioscopy. The first phase was from October 2001 to September 2002, the second was from October 2002 to September 2003 and the final phase was from October 2003 to February 2005.
Population
One hundred and fifty-seven patients with dilated cardiomyopathy were studied with ages between 26 and 84 years (average age from 55 ± 16 years). Sixty-eight (43.5%) of the patients were female and 89 (56.5%) male. Fifteen (9.8%) patients presented permanent atrial fibrillation and 16 (10.5%) patients had definitive pacemakers previously implanted for the treatment of bradyarrhythmias.
Inclusion criteria
The inclusion criteria were: 1) patients with dilated cardiomyopathy (DCM) and functional class III congestive heart failure (NYHA) or IV refractory to the optimized medicinal therapy; 2) patients with DCM in which there was no possibility of surgical repair (myocardial revascularization, valve replacement, left ventricular aneurysm resection or congenital heart diseases); 3) patients without primary indication for the reestablishment of heart frequency or of atrioventricular synchronism; 4) exteriorized interventricular conduction disorders such as left branch or right branch standard blocks associated with antero-superior divisional or left branch block exclusively induced by right ventricular heart pacing; 5) duration of the QRS complex greater than or equal to 130 ms.
Exclusion criteria
1) Infarction or unstable angina in the previous three months; 2) acute myocarditis; 3) pregnancy and 4) drug addiction or alcoholism.
Surgical procedure
All procedures were performed under local anesthesia and when necessary under sedation, depending on the degree of congestive heart failure and on the tolerance to an extended time in the decubitus position. Patients received prophylactic intravenous antibiotics one hour before the procedure. They were placed in the horizontal dorsal decubitus position, with electrocardiographic monitoring with all the electrodes positioned on the right hemi-thorax when the surgery was performed on the left (gold standard), or left when the surgery was performed on the right (in cases in which it is impossibility to implant on the left side or when the patient already had a definitive pacemaker implanted on the right), so that all the electrodes were far from the heart image (two leads in the right deltoid region, anterior and posterior and one lead on the anterior-left axillary line in the seventh intercostal space). The D2 bipolar derivation was utilized and the active lead was always placed in the deltoid region.
The first lead was placed in the right ventricle (RV), followed by the right atrium lead, both, when possible, through the left cephalic vein. When it was impossible to pass one or both the leads, a new venous puncture was performed in order to obtain a passage. These leads (active) were placed in the traditional sites (atrium lead in the right auricula and the right ventricle lead at its tip) or where initiation of stimulation, sensitivity and acceptable impedance were identified. In the cases in which there were indications for the implantation of associated implantable cardioversion-defibrillators (ICD), passively fixed double spring leads were utilized, placed at the tip of the right ventricle. In patients with previously implanted double chamber pacemakers, only a puncture for the left ventricular pacing lead was made. The last lead to be placed was the coronary sinus lead to stimulate the left ventricle. In our study Aescula 1055K (St. Jude Medical), Attain 2187 or 4193 (Medtronic) and Corox+LV-H or Corox OTW (Biotronik) leads were utilized. This lead was passed into the subclavian vein and catheterization of coronary sinus was obtained following a radiological image of the anatomy using fluoroscopy from a left anterior oblique view, at an angle of 35 degrees and unipolar intracavitary electrography obtained by connecting the coronary sinus lead to the guide lead of the electrocardiographic monitoring (Figure 1).
The lead was adjusted in compliance with the anatomy of right atrium. Its adaptation was achieved by shaping its guide wire (Figure 2).
After shaping, the lead was placed in the low atrial septum region. In this position, the lead was moved slightly to the top and bottom (utilizing radiologic anatomy), forwards and backwards, by anti-clockwise and clockwise rotation, respectively (utilizing intracavitary electrography). Regions near to the atrioventricular ring gave well-defined electrograms with the presence of both atrial and ventricular components.
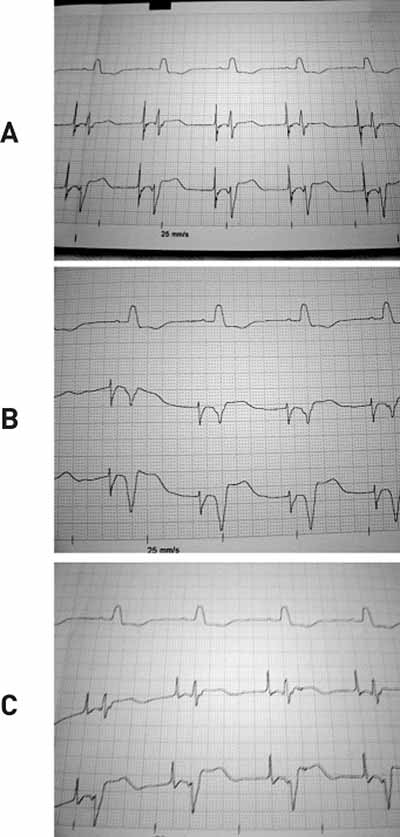
In patients who presented with sinusal rhythm, the atrial component in the region of the coronary sinus ostium was isodiphasic (Figure 3A). The more the lead went backwards and distant from the CS ostium, the atrial component became progressively more negative (Figure 3B). On the other hand, the more the lead came forwards and distant from the ostium, the atrial component became progressively positive (Figure 3). In this situation, it was not rare to pass through the tricuspid valve and migrate to the ventricle, creating high ventricular potentials, eventually inducing non-sustained ventricular tachycardia.
It is known that the right atrial intracavitary electrogram presents different morphologies and components that are dependent on the arrangement of the leads in its different anatomical regions. High regions of the right atrium present with predominantly negative potentials, mid-regions of the right atrium present isodiphasic potentials and low regions of the right atrium present predominantly positive potentials [12] (Figure 4 A, B and C).
After catheterization of the coronary sinus ostium the lead was placed in a tributary vein of the coronary sinus, utilizing the shape of the guide utilized for the catheterization of the ostium or in specific cases a new guide wire in an "S" shape was introduced into the lead, facilitating its placement. The choice was made with preference to left ventricle lateral and posterior wall veins, followed by the stability of the catheter, absence of diaphragmatic pacing with maximum pacing of 10 Volts, sensitivity pacing thresholds and impedance of left ventricle and biventricular, in cases of generators without independent exits.
RESULTS
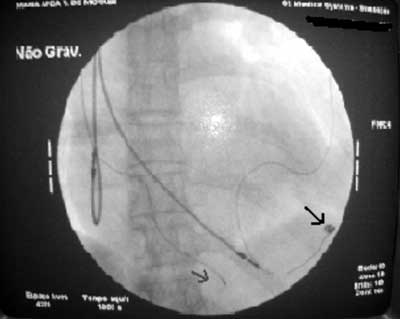
Left ventricular pacing was successfully obtained in all patients. In 11 patients left ventricular pacing was not obtained using the transvenous method as the first surgery, in sixpatients because of the impossibility of catheterization of the coronary sinus and in five patients because of a placement error in one of the tributaries of the coronary venous sinus. These patients were immediately submitted to the implantation of epimyocardial leads by thoracotomy. Five of the patients submitted to epimyocardial lead implantation presented, after a mean time of 29.4 ± 4.6 months, excessive increases in the electrode command threshold for left ventricular pacing. They were submitted to re-interventions to attempt transvenous pacing again and this time success was obtained in all five cases (Figure 5).
The catheterization of the coronary vein with the utilization of the radiologic anatomy and intracavitary electrogram was successfully performed in 150 procedures. At the moment of the catheterization of the coronary sinus ostium in patients who presented sinusal rhythm (136 patients), the atrial component was seen to be isodiphasic in 133 (97.7%) of them and predominantly positive in three (2.3%) patients. The placing of the lead in coronary sinus tributaries was successful in 145 (92.9%) procedures, with an average time of radioscopy of 18.27 ± 15.46 minutes. The success rate progressively increased with the experience of the surgeon. In the first phase of observation, the success rate was of 55.5% with an average time of radioscopy of 43.6 ± 18.6 minutes, in the second phase it was of 92.6%, with a mean time of 18.14 ± 13 minutes and in the third phase it was 98.2%, with an average time of 13.76 ± 4.66 minutes. In five patients, in which cannulation of the coronary sinus was obtained, the placement of the leads was not successful: in four cases due to the difficulty of placing the lead in a tributary of the coronary venous system and, consequently, it was impossible to have acceptable thresholds and in one patient due to diaphragmatic stimulation in the only place in which it was possible to achieve stimulation of the left ventricle. In eleven procedures, pacing of the left ventricle was obtained through the implantation of epimyocardial leads by thoracotomy.
Difficulty in cannulating the coronary sinus was experienced in 20 patients, in spite of the adequate intracavitary potentials and the placement using radiological imaging. In six cases maneuvers of the lead and guide wire were performed enabling the passage of the lead through the ostium and the lead was placed in the coronary sinus. In eight cases, a stiffer guide wire with sharper curves was utilized thereby assisting the passage of the lead. In 39 patients we had difficulty with the insertion of the lead, probably where the great cardiac vein drains into the coronary sinus. This problem was solved in 30 procedures by successive movements of the electrode and its guide wire. In nine cases, another straighter and more rigid guide replaced the pre-shaped guide. In 12 cases the electrode had to be repositioned after removal of the guide accidental displaced it. Ten patients presented diaphragmatic stimulation and the electrode was successfully repositioned in nine patients. Three patients presented transitory total atrioventricular blocks after manipulation of the electrode in the right ventricular cavity, making temporary ventricular pacing necessary. In three cases, there was displacement of the atrial electrode during manipulation of the coronary sinus electrode, making its repositioning necessary.
In two cases, the left side implantation was interrupted and the leads were successfully implanted from the right; one was because of the impossibility of advancing the electrodes up to the right cavities due to the presence of persistent left vena cava and narrow coronary sinus, making the passage of the three electrodes impossible through the same access route.

Fig 1 - Photo demonstrating the procedure to achieve the unipolar intracavitary electrogram. Observe that the distal annulus of the electrode is connected to the explorer electrode by means of a lead.

Fig. 2 - Guide wires with different formats (curves of different sizes and shapes) to adapt to the variations in the size and anatomy of the atria.
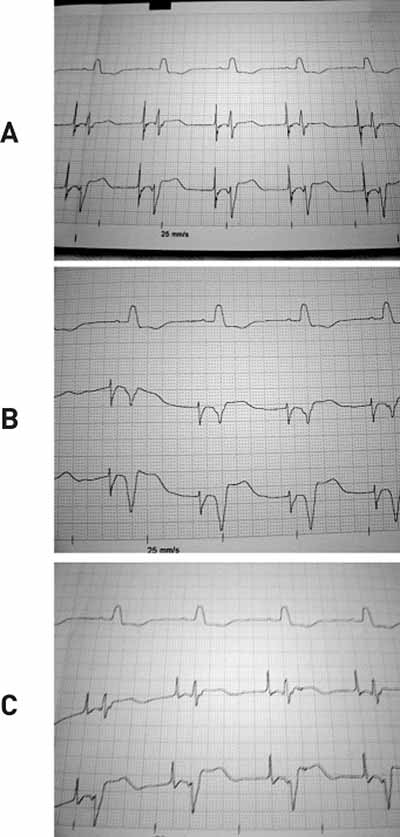
Fig. 3 - The upper trace shows a surface electrocardiogram of 25 mm/s. The lower traces show unipolar intracavitary electrograms obtained during the procedure, with an electrode placed in the right postero-septal region. (A) Intracavitary electrogram obtained in the coronary sinus ostium. (B) Electrogram obtained near to, but in regions behind the coronary sinus ostium. (C) Electrogram obtained, near to, but in regions in front of the coronary sinus ostium.

Fig. 4 - Diagram illustrating the right atrial cavity, demonstrating the position of the electrode in the high, middle and low regions of the right atrium and the resultant vector of depolarization. To the left is a diagram showing the intracavitary electrogram obtained in the three situations. (A) Electrode placed in the region behind the coronary sinus ostium (high right atrium). (B) Electrode placed in region of the coronary sinus ostium (middle right atrium). (C) Electrode placed in the region in front of the coronary ostium sinus (low right atrium). (CS= coronary sinus ostium), FO= fossa ovalis, LCV= inferior vena cava, UVC= superior vena cava, VAN = ventricular atrial node, ASN = atrial sinal node, RA= right atrium.
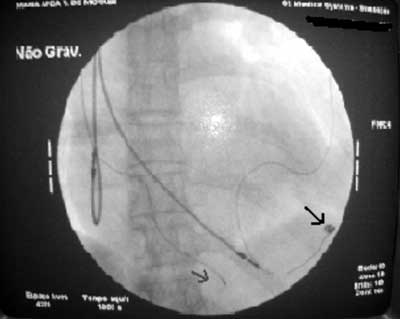
Fig. 5 - Radioscopic image of the left anterior oblique position of a patient who was submitted to a reintervention of transvenous left ventricle pacing. Observe the black arrow showing an abandoned epicardial electrode and the red arrow showing the transvenous electrode placed in the posterior region of the left ventricle.
COMMENTS
Cardiac resynchronization therapy has demonstrated good results in the treatment of pre-selected patients with congestive heart failure [1-3]. The traditional method of lead implantation for left ventricular pacing is epimyocardial by lateral or subxiphoid thoracotomy or by thoracoscopy. These methods have already been demonstrated as efficient and were routinely used before the invention of transvenous electrodes for epicardial pacing with endocardial [13]. The main obstacles to the routine epimyocardial implantation of leads for left ventricular pacing in patients with enlarged cardiomyopathy and congestive heart failure are the risks associated with general anesthesia and post-surgical morbidity [14]. Currently, the transvenous method using an endocardial access is the gold standard because it reduces the complexity of the surgery and, consequently, its morbidity and time of hospital stay [7].
One of the main limitations of the application of the transvenous technique is the catheterization of the coronary sinus and the placement of a special electrode in one of its tributaries for left ventricular pacing [5,13]. The success of the implantation depends on multiple variables, including experience and technique of the surgeon, anatomy of the coronary sinus and availability and variety of special materials [6].
In spite of the great advances in technology and evolution in the implantation techniques using sheaf systems, special systems of guide wires such as side-the-wire [11] and over-the-wire [8, 13], or proposals of coronary sinus cannulation guided by electrophysiologic catheters [7] have been demonstrated to be efficient. Even so the proposed techniques, whether by sheaf associated with contrast, special guide wires or inadequate intracavitary electric signals, still only utilize radiologic anatomy and a series of trials and errors when cannulating the coronary sinus. Taking into account this limitation which still remains, the authors present the experience of just one center, of a technique that attempts to facilitate the cannulation of the coronary sinus based on the radiologic imaging of the anatomy and intracavitary electrogram, emphasizing the atrial electrogram morphology of patients who present with sinusal rhythm.
The choice of the left side for the procedure was due to two reasons. Firstly, because of the facility of routing the lead to the site of the pacemaker in cases in which the pacing had to be epimyocardially performed by thoracotomy. The second is that, eventually, patients present with a persistent left vena cava with atresia of the coronary sinus ostium [14,15], making implantation to the right impossible. We chose to implant conventional electrodes for right ventricular and atrial pacing, respectively, as they serve as points of anatomical definition and because, during the manipulation of the electrode in the patients with blocks of the left branch, there is a risk of injury to the right branch, causing total atrioventricular blocks and the necessity of temporary cardiac pacing, as has been described in the literature [6] and which occurred in two of our patients.
With the utilization of the radioscopy using a left anterior oblique (LAO) view at 35º, a bidimensional anatomical relationship between the tricuspid and mitral annuli was obtained, clearly demonstrating the lateral and septal walls of the right atrium. With the help of the intracavitary electrogram, we identified the proximal regions of the atrioventricular annulus, demonstrating atrial and ventricular intracavitary electrograms with ratios of 1:2 or less [16]. It is known that the coronary sinus ostium is in the right postero-septal or proximal regions, or even in the atrioventricular annulus itself, the electrode was placed in this region by utilizing the guide wire of the electrode which had previously been shaped, while watching the atrial and ventricular electrogram.
Manipulation of upper and lower regions was easily performed using the radiologic anatomy. However, the radioscopy provided bidimensional images and consequently mobilization in the anterior and posterior regions could not be controlled by it. Thus, these movements of the electrode were accompanied based on the atrial component of the intracavitary electrogram in patients with sinusal rhythm. It was observed that, in the coronary sinus ostium, from where it was possible to catheterize the coronary sinus, the intracavitary electrogram was seen to be isodiphasic in 133 of the 136 procedures, in which patients were in sinusal rhythm and catheterization of the coronary sinus was possible. In these patients it was still observed that a slight movement of the electrode to the posterior region turned the atrial component predominantly negative, and that displacement to the anterior region made it predominantly positive, positions that were checked with the radioscopy in right anterior oblique (RAO) view. A possible explanation for these observations was found: it is known that the resulting vector of the right atrial depolarization initiates in the sinusal-node region and is directed downwards, forwards and a little to the left [15,17].
As the coronary sinus ostium is in the posterior region of the right atrium, in front of and to the side of the lower vena cava valve and in front of the septal cuspid of the tricuspid valve [18], this is, due to its anatomic position, perpendicular to the vector of atrial depolarization. As the atrial electrogram obtained with the electrode is unipolar, the placement of this on the coronary sinus ostium would put it in an almost vertical position creating isodiphasic potentials [17]. In this situation, moving the electrode backwards, the electrode would tend to observe the tail of the vector, and the signal would become more negative and, forwards observing the tip of the vector, the signal would become more positive [17], as demonstrated in the Figure 4.
Galvão Filho [12], in 1990, also demonstrated that the atrial electrogram varies according to its location in the right atrium. However, he utilized a different manner to explain the anatomic structure of the right atrium based on a bidimensional image from the author. What Galvão Filho denominated as high right atrium and low right atrium correspond to the upper and lower regions (close to the tricuspid ring) of the right atrium. In the radiological anatomy utilized by the authors (left anterior oblique view), posterior regions to the coronary sinus ostium correspond to the upper region of the right atrium and anterior regions to the coronary sinus ostium correspond to the lower region.
Our success rate of 94.4% was similar to published rates [6-8] and clearly showed a learning curve with a success rate in the first year of 55.5% and 98.2% in the last year. The European register of CONTAK revealed with details that the average duration of the procedure and the success rate was directly proportional to the experience of the surgeon [8]. Surgeons that performed more of 20 implantations achieved the procedure in shorter times associated with shorter times utilizing the radioscopy. The average time of implantation was 90 ± 38 minutes with a radioscopy time of 27 ± 21 minutes. Our total average time of radioscopy was 18.21 minutes. Compared to the literature, our total average time of radioscopy was shorter than those cited by Kautzner et al. [6], Butter et al. [10], Purerfellner et al. [7] and Yee et al. [19]. This can be explained by the fact that many surgeons were involved in these works and, in some cases, many centers, thus the results were influenced by the experience of each individual surgeon. In our work, the results were influenced by the learning curve of only one surgeon. Also, in this study, the sheaf was not utilized for catheterization of the coronary sinus instead it was directly cannulated with an electrode itself, thus reducing the chances of displacement with the removal of the sheaf which consequently increases the time of the procedure [4].
Analyzing, the intra-operative difficulties in 20 procedures we experienced difficulties in the cannulation of the coronary sinus ostium. In six procedures, the cannulation was not possible and, in five patients, the placement of the electrode in one of its tributaries was not possible, demonstrating the importance of the anatomic variations of the coronary sinus ostium [6], of the angle and of the caliber of its tributaries, and even the presence and anatomy of a Thebesios' valve, in the catheterization of the coronary sinus. In one study of 143 patients, 62.9% presented the valve; in 73 patients the valve had a semi-lunar shape, in 10 cases a septal shape and in seven cases a shape like a crest [20]. In 39 procedures, there were difficulties with the forward movement of the electrode through the coronary venous sinus, near to the junction of the great cardiac vein, a probable location of the Vissencius' valve as found in 87% of the studied cases by Lundinghausen et al. [21], also demonstrating the importance of this valve in the implantation procedure of the coronary sinus electrode.
Conclusion
The implantation technique employed by the author, that utilizes intracavitary electrogram and radiological anatomy, proved to be safe and efficient for the cannulation of the coronary sinus ostium and its placement in one of its tributaries with a short radioscopy time.
BIBLIOGRAPHIC REFERENCES
1. Aurichio A, Stellbrink C, Sack S et al. Chronic benefit as a result of pacing in congestive heart failure: results of the PATH-CHF trial. Circulation. 2000;102:3352A.
2. Linde C, Leclercq C, Rex S, Garrigue S, Lavergne T, Cazeau S et al. Long-term benefits of biventricular pacing in congestive heart failure: results from the MUltisite STimulation In Cardiomyopathy (MUSTIC) study. J Am Coll Cardiol. 2002;40(1):111-8.
3. Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346(24):1845-53.
4. Fatemi M, Etienne Y, Gilard M, Mansourati J, Blanc JJ. Short and long-term single-center experience with an S-shaped unipolar lead for left ventricular pacing. Europace. 2003;5(2):207-11.
5. Curnis A, Neris R, Mascioli G et al. Left ventricular pacing lead choice base on coronary sinus venous anatomy. Eur Heart J. 2000;2(Suppl J):J31-5.
6. Kautzner J, Riedlbauchová L, Cihák R, Bytesnic J, Vancura V. Technical aspects of implantation of LV lead for cardiac resynchronization therapy in chronic heart failure. Pacing Clin Electrophysiol. 2004;27(6 pt 1):783-90.
7. Purerfellner H, Nesser HJ, Winter S, Schwierz T, Hornell H, Maertens S. Transvenous left ventricular lead implantation with the EASYTRACK lead system: the European experience. Am J Cardiol. 2000;86(9 suppl 1):K157-64.
8. Neuzner J, Pappone C, Aurichio A et al. Learning curve for the first 1000 over-the-wire left ventricular transvenous lead implants-a Europe experience. Eur J Heart Failure 2001;3(suppl.1):S13.
9. Curley J, Lamba S, Moulton K et al. Does the availability of left heart lead and delivery system options matter for cardiac resynchronization therapy? Pacing Clin Electrophysiol. 2002;24(Pt. II):597.
10. Butter C, Gras D, Ritter P, Stellbrink C, Fleck E, Tockman B et al. Comparative prospective randomized efficacy testing of different guiding catheters for coronary sinus cannulation in heart failure patients. J Interv Card Electrophysiol. 2003;9(3):343-51.
11. Walker S, Levy T, Rex S, Paul VE. The use of a "side-wire" permanent transvenous-pacing electrode for left ventricular pacing. Europace. 1999;1(3):197-200.
12. Galvão Filho SS. Passagem de cabo eletrodo para estimulação cardíaca artificial provisória, orientada por monitorização endocavitária. An Paul Med Cir. 1990;117(1,2):47-53.
13. Auricchio A, Klein H, Tockman B, Sack S, Stellbrink C, Neuzner J et al. Transvenous biventricular pacing for heart failure: can the obstacles be overcome? Am J Cardiol. 1999;83(5B):136D-42.
14. Santoscoy R, Walters HL 3rd, Ross RD, Lyons JM, Hakimi M. Coronary sinus ostial atresia with persistent left superior vena cava. Ann Thorac Surg. 1996;61(3):879-82.
15. Jha NK, Gogna A, Tan TH, Wong KY, Shankar S. Atresia of coronary sinus ostium with retrograde drainage via persistent left superior vena cava. Ann Thorac Surg. 2003;76(6):2091-2.
16. Niebauer MJ, Daoud E, Williamson B, Man KC, Strickberger A, Hummel J et al. Atrial electrogram characteristics in patients with and without atrioventricular nodal reentrant tachycardia. Circulation. 1995;92(1):77-89.
17. Carneiro EF. A ativação do coração. In: O eletrocardiograma - 10 anos depois. Rio de Janeiro:Cervantes Editora;1997.
18. Warwickshire: General Practice Notebook - a UK medical encyclopedia on the World Wide Web; c2004. Disponível em: http://www.gpnotebook.co.uk [acessada em 1/12/2004].
19. Yee R, Pappone C, Maertens S et al. Clinical experience with over-the-wire left ventricular pacing lead for biventricular pacing in heart failure patients: multicenter report. Can J Cardiol. 2001;(suppl C):89C-288C.
20. Bergman RA, Afifi A, Miyauchi R. Coronary Sinus. In: Anson BJ, editor. Illustrated encyclopedia of human anatomic variation: Opus II: cardiovascular system: veins: head, neck, and thorax. 12ª ed. New York:McGraw-Hill;1966.
21. Lundinghausen M, Ohmachi N, Boot C. Myocardial coverage of the coronary sinus and related veins. Clin Anat. 1992;5:1-15.



 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license