INTRODUCTION
Coronary artery Spasms (CAS) are rare but may occur as a severe complication in the coronary artery bypass surgery (CABS) and are seen as an important cause of acute myocardial infarction (AMI) in the intra-operative and immediate postoperative periods (IPO) [1-3].
The small number of published cases makes treatment and recognition of risks associated to this complication difficult [2].
In this work, we present the case of a patient who was submitted to on-pump coronary artery bypass surgery who presented with positive deflection of the ST segment suggestive of AMI in the immediate postoperative period, when a heart catheterism (CAT) was performed demonstrating CAS. Included is a concise review of the literature.
CASE REPORT
A 47-year-old female patient presented typical precordial pain over a three-month period. She arrived in the hospital emergency department with a strong precordial pain, cold sudoresis, vomits and hypotension. After a physical examination and echocardiography, AMI was diagnosed with positive deflection of the ST segment from V1 to V4, D1 and AVL. The patient evolved with hemodynamical instability, followed by cardiorespiratory arrest and was successfully revived. After spontaneous return of the circulation, the use of thrombolytic agents was opted for. Her clinical evolution was good and she was discharged on the 7th day after hospitalization.
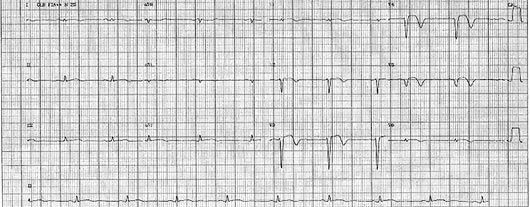
After the acute phase, echocardiography showed non-specific ventricular depolarization, as well as left branch blockade (Figure 1 A). A hemodynamical study performed during hospitalization indicated injury to the right coronary artery (RC) of 70%, ulcerated plaques in the anterior descending (AD) and circumflex (CX) arteries of approximately 95% and 50%, respectively, and the left ventricle presented apical paralysis and inferior hypokinesia, indicating the need for elective surgical treatment.
The surgery was performed by medium sternotomy, with cardiopulmonary bypass lasting 85 minutes and anoxia for 40 minutes. Systemic hypothermia at 28 ºC was established with myocardial protection using a hypothermic anterograde blood cardioplegic solution at intervals of 20 minutes with warmed reperfusion. Distal anastomoses of the left internal thoracic artery to the AD and saphenous grafts to the RC and the left marginal arteries were performed. During surgery normal calibers of coronary arteries and the presence of diffuse atherosclerotic plaques were observed.
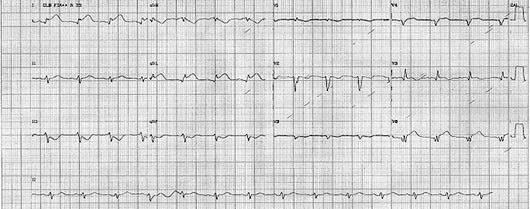
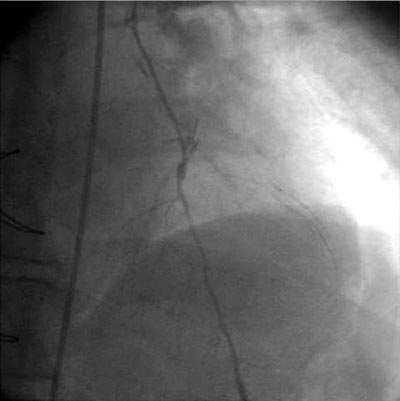
After admission to the intensive care unit the patient presented alterations of the echocardiogram with a positive deflection of the ST segment at V1 and AVL, together with negative deflection of the ST segment at DIII (Figure 1B), followed by hemodynamic instability. Treatment with vasoactive drugs (noradrenaline) and an increase in the coronary vasodilator dose were chosen, but without improvement of the hemodynamic state or the electrocardiogram. The patient was then submitted to cinecoronariography which demonstrated spasms of the AD (Figure 2 A) but with all grafts pervious. At this moment, administration of intracoronary vasodilators was opted for giving a good clinical response with restitution of the primitive arterial caliber (Figure 2B).
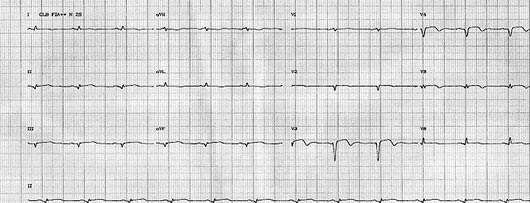
Hemodynamic stabilization and normalization of the ECG (Figure 1C) occurred. The patient was discharged from the ICU on the 2nd postoperative day and from hospital on the 8th postoperative day. The patient evolved well and is asymptomatic eight months after the operation.
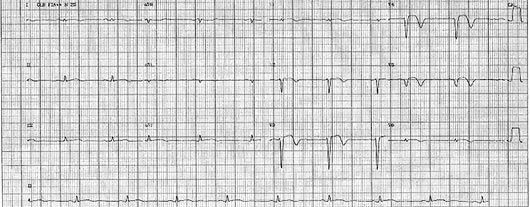
Fig. 1A - Preoperative period
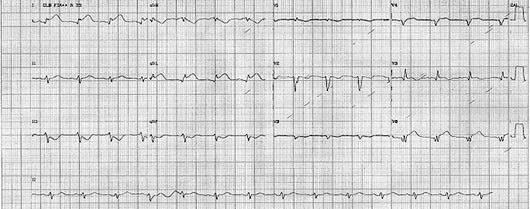
Fig. 1B - Immediate postoperative period before re-study
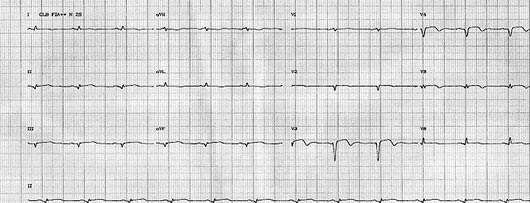
Fig. 1C - 1st postoperative period

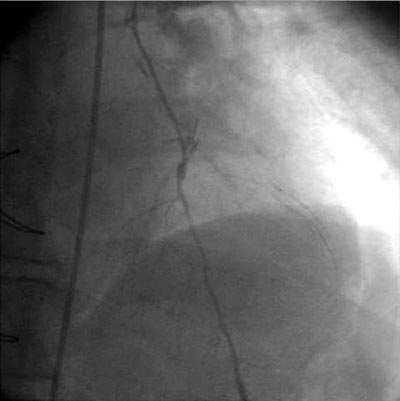
Fig. 2A - Anterior descending artery with spasm. Contrast injected in the left internal thoracic artery. 2B - Anterior descending artery after injection of coronary vasodilators in the left internal thoracic artery
The sudden appearance of hemodynamic instability in the immediate postoperative period of CABS may be caused by CAS [1,2] with characteristics including a sudden onset of hypertension associated with arrhythmias or not, occasionally bradycardia, widening of the QRS complex or positive deflection of the ST segment and, in the majority of cases, good response to intravenous or intracoronary vasodilators [1,2].
The mechanism of CAS has been known for a long time go. In 1959, Prinsmetal described for the first time a type of reversal angina caused by changes in the coronary vagal tonus [3]. In 1972, Bentivoglio reported AMI caused by CAS in 22 patients, but without angiography confirmation [3]. In 1977, Oliva et al. confirmed CAS angiographically [3]. Several authors published similar reports, but none of them managed to establish a causal relation between CAS and ischemic events [3]. Does AMI occur before or after the spasm? This question is difficult to respond as there are few studies that demonstrate this relationship. Vicente et al. demonstrated angiographically a case of CAS preceding the thrombotic event of AMI [4].
There are several factors that may predispose patients to CAS in the intra- and postoperative periods of heart surgeries including the existence of coronary atheromatosis. There are reports in the literature of CAS in apparently normal coronary arteries [4]. The excessive use of vasoconstrictor agents has also been correlated to a higher incidence of spasms. Other factors related to CPB or to the surgical procedure used increase the incidence of events, including cooling of the patient and the excess of calcium and potassium used in cardioplegic solutions. Other factors related to tissues such as endothelial injury and the actions of serotonin and endogenic histamine may also influence the genesis of CAS [1].
The incidence of CAS is more common among Asiatic individuals than Caucasians [2]. Koshiba et al. [2] studied the clinical-surgical profile of 115 cases of CAS related to heart surgery. The average age of the patients was 64 years, with 94% of the cases over 50 years old. Men were the most affected (84%). In respect to risk factors, systemic arterial hypertension, prior angina and smoking were the commonest. Most events were identified in the intraoperative period (76%) with 11% in the immediate postoperative period. Other factors that can contribute are inadequate anesthesia (23%), vasopressor agents (22%) and mechanical stimulation, among others.
A previous angiographic diagnosis must be made in the course of CAS refractory to medicinal therapy with the aim of obtaining the exact diagnosis [3]. CAS is normally found in only one vessel, but may occur in several arteries simultaneously [4,6].
The treatment of CAS must be individualized and adapted to clinical conditions and may range from conventional therapy with nitrates and calcium channel antagonists to mechanical support or re-establishment of CPB, when diagnosed during surgery [1-6].
In this case, the presence of severe and diffuse coronary injury, hypothermia in the intraoperative period, the use of potassium in the cardioplegic solution and the handling of the AD to perform anastomoses, may have been the involved risk factors, considering the extensive arterial involvement. The criteria used to submit patients who evolve with AMI in the immediate postoperative period to angiographic study, can define the diagnosis and adequate treatment. After the CAT, infusion of vasodilator agents was maintained as described in the literature [1,3,6]. We routinely employ calcium channel blockers to patients who will be submitted to CABS with the use of grafting of the radial arterial, a conduct that might be extended to cases with higher risks of CAS.
In conclusion, CAS has a multifactorial character, sudden appearance and frequently improves with the administration of intravenous nitrates and calcium channel blockers. It must be included in the differential diagnosis as a cause of AMI and low output syndrome in patients who were submitted to heart surgeries.
BIBLIOGRAPHIC REFERENCES
1. Kinoshita, Matsuzaki K, Mayumi H, Asou T, Masuda M, Kawachi Y et al. A new aspect of coronary artery spasm induced by cardiac surgery. Jpn J Surg. 1991;21(4):395-401.
2. Koshiba K, Hoka S. Clinical characteristics of perioperative coronary spasm: reviews of 115 case reports in Japan. J Anesth. 2001;15(2):93-9.
3. Freedman RJ, Fuentes F, Smalling RW, Kirkeeide RL, Sterling RP,Walker WE et al. Left coronary artery spasm causing severe left ventricular dysfunction without myocardial infarction. Texas Heart Inst J. 1986;13(2):223-31.
4. Takashiba K, Matsuda Y, Hamada Y, Ohno H, Hyakuna E, Fujii M et al. Recurrence of myocardial infarction related to different vessels in a patient with diffuse coronary artery spasm without underlying severe organic stenosis. Clin Cardiol. 1988;11(4):265-7.
5. Sakuma M, Kamishirado H, Inoue T, Ichihara K, Takayanagi K, Hayashi T et al. Acute myocardial infarction associated with myocardial bridge and coronary artery vasospasm. Int J Clin Pract. 2002;56(9):721-2.
6. Cipriano PR, Koch FH, Rosenthal SJ, Schroeder JS. Clinical course of patients following the demonstration of coronary artery spasm by angiography. Am Heart J. 1981;101(2):127-34.

 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license