INTRODUCTION
Primary intracardiac tumors are an extremely rare condition with the majority of reported cases being benign tumors; 50% of which are myxoma, whilst 5 to 10% of these tumors are hemangiomas as has been reported in several surgical series. In many cases, the hemangiomas are asymptomatic, discovered by chance at necropsy or during heart surgery for another associated disease. In symptomatic patients, hemangiomas may simulate valve diseases, be related to arrhythmias, pulmonary congestion, or even be associated to sudden death, according to their location. We report on a case of a hemangioma in the left atrium associated to dyspnea, which was surgically excised, from a schistosomotic patient with significant hypersplenism.
CASE REPORT
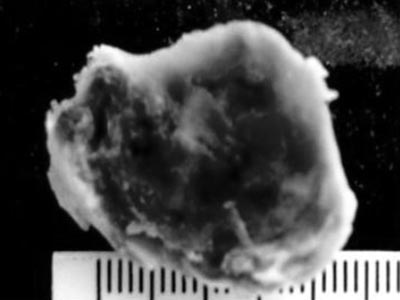
A 49-year-old woman, with schistosomotic hepatosplenomegaly developing to portal hypertension and esophageal varicose veins under clinical-surgical management, was referred for cardiological evaluation due to dyspnea on moderate effort. On examination the patient was normotensive; the heart rhythm was regular, the heart noises were normal with systolic/diastolic murmurs (1+/6+) in the mitral region. Chest radiography showed her heart area was slightly increased (1+/4+). Electrocardiogram indicated sinusal rhythm with signs of chamber overload. A Doppler echocardiogram showed the left atrium was dilated with an image of a mass adhered to its medial wall suggesting myxoma but without evidence of pulmonary hypertension. The patient was submitted to a hemodynamic study, which evidenced a nodule in the left atrium, near to the implantation of the mitral valve, which was fixed and slightly calcified (probable myxoma) - Figure 1: mild hypertension in the pulmonary artery as well as discrete diffuse coronary atherosclerosis and the left ventricle with discrete diffuse hypokinesia.
Laboratory examinations showed significant persistent thrombocytopenia (54,000/mm3). The patient was referred for hematologic evaluation and was submitted to a myelogram, which identified an increased number of megakaryocytes, with diminished platelet production, compatible with hypersplenism. A cardiovascular surgical procedure was indicated after preoperative preparation that included preparation of platelet for transfusion.
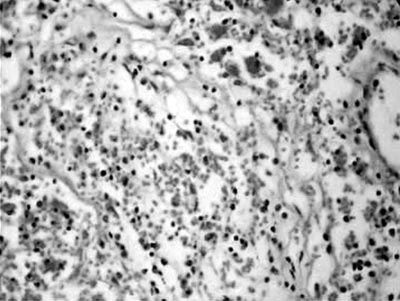
The surgical procedure was performed under cardiopulmonary bypass (CPB) support. After left atriotomy, a clear nodular and encapsulated tumoral mass was observed in the left atrial roof. Resection was performed and the region was submitted to electrocauterization. The CPB was weaned after the spontaneous return of heartbeats. The CPB time was 35 minutes at a temperature of 34 ºC. During closure of the chest, thorough hemostasis was performed. The resected material was sent for anatomopathological study that revealed it to be a pale smooth, nodular mass with a focal point of calcification of 2.5 cm in diameter, with hemorrhagic areas evidenced in the sections (Figure 2a.) Microscopy showed a benign lesion with a hyalinized area with capillary vascular proliferation lined by endothelium as well as presence of thick-walled blood vessels with calcified focal points (Figure 2b). Atypical cells or myxoid tissues were not evidenced suggesting a benign capillary hemangioma.
The patient presented significant bleeding in the first hours of the postoperative period, requiring blood transfusion including replacement of platelets to control the bleeding after the third hour. From then on she presented with a good postoperative evolution and was released from the intensive care unit on the second postoperative day and from hospital on the ninth postoperative day, without further adverse events. Thenceforth, she continues under clinical-cardiological control, showing a good evolution and has been referred for clinical-surgical and hematological management of the hypersplenism.

Fig. 1 - Hemodynamic study showing the hemangioma
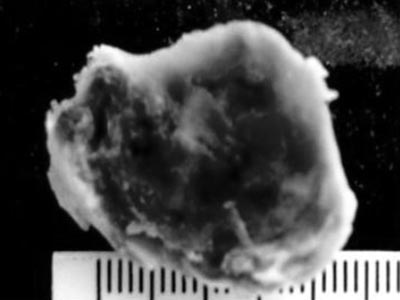
Fig. 2A - Hemangioma - macroscopic appearance
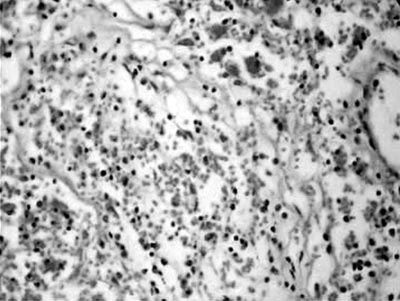
Fig. 2B - Hemangioma - microscopic appearance
Primary intracardiac tumors are extremely rare, with an incidence of from 0.001 to 0.3% with benign tumors in approximately 75% of these cases. Myxomas are the commonest type of tumors (approximately 50%), with from 5 to 10% being hemangiomas as reported by several surgical series [1,2]. Hemangiomas are histologically characterized in 3 types: cavernous (formed by multiple, dilated vessels with thin walls), capillary (formed by small vessels resembling capillaries) and arterial-venous (formed by small arteries and dysplasic veins). Heart hemangiomas frequently combine criteria of the three histological types, as well as fibrous tissue and fat cells. Around 15% of hemangiomas involve the pericardium or epicardium.
Hemangiomas occur at any age, but the diagnosis predominantly occurs in the fourth decade of life [3,4]. In reported surgical series, there is a predominance of male patients (around 65%). In many cases the hemangiomas are asymptomatic, discovered by chance at necropsy or during heart surgery for other associated diseases. In symptomatic patients, hemangiomas may be related to arrhythmias, pulmonary congestion, heart failure, obstruction of the left or right ventricle outflow tracts or coronary failure, and may even be associated to sudden death, when there is an associated to conduction disorders, attributable to the proximity of the hemangioma to the AV node or to a ventricular location.
A rare mechanism of sudden death in individuals with heart hemangioma is the rupture of the tumor in the pericardial cavity, with subsequent tamponade. There is a rare association of heart hemangiomas with gastrointestinal tract hemangiomas [3] or port-wine-stain-type facial hemangiomas. Giant hemangiomas may even be related to thrombosis or coagulopathies (Kasabach-Merritt) [5].
Heart hemangiomas may exist in varied locations. In several previously reported series, approximately 34% were found in the atria, 27% in the left ventricle or interventricular septum, 24% in the right ventricle, 13% in the pericardium or epicardium and 2% in the mitral valve [4]. In the current report, the patient had persistent thrombocytopenia, secondary to schistosomotic hepatosplenomegaly with clinical compatibility of mitral valve disease, but a diagnosis suggestive of left atrial myxoma was made by imaging techniques (echocardiogram and hemodynamic study). The patient was submitted to surgery to excise the tumor which was subsequently sent for anatomopathological study giving a histological definition and diagnosis of the disease. The patient presented a hemorrhage in the immediate postoperative period but responded well to blood transfusions and platelet replacement.
The study of predisposing factors for the bleeding after heart surgery [6], with an increase of the transfusional requirements, is related to preoperative thrombocytopenia and CPB use (mainly prolonged CPB with hypothermia). In the present report, the increased bleeding, attributed principally to the thrombocytopenia with aggravation due to the use of CPB (although for a short time and without deep hypothermia), was corrected with platelet replacement. The patient presented good evolution since then, without other adverse events.
BIBLIOGRAPHIC REFERENCES
1. Dein JR, Frist WH, Stinson EB, Miller DC, Baldwin JC, Oyer PE et al. Primary cardiac neoplasms. Early and late results of surgical treatment in 42 patients. J Thorac Cardiovasc Surg. 1987;93(4):502-11.
2. Murphy MC, Sweeney MS, Putnam JB, Walker WE, Frazier OH, Ott DA et al. Surgical treatment of cardiac tumors: a 25-years experience. Ann Thorac Surg.1990;49(4):612-8.
3. Burke A, Johns JP, Virmani R. Hemangiomas of the heart: a clinicopathologic study of ten cases. Am J Cardiovasc Pathol. 1990;3(4):283-90.
4. Abad C, Campo E, Estruch R, Condom E, Barriuso C, Tassies D et al. Cardiac hemangioma with papillary endothelial hyperplasia: report of a resected case and review of the literature. Ann Thorac Surg. 1990;49(2):305-8.
5. Gengenbach S, Ridker PM. Left ventricular hemangioma in Kasabach-Merritt syndrome. Am Heart J. 1991;121(1 pt 1):202-3.
6. Miana LA, Atik FA, Moreira LF, Hueb AC, Jatene FB, Auler Junior JO et al. Fatores de risco de sangramento no pós-operatório de cirurgia cardíaca em pacientes adultos. Rev Bras Cir Cardiovasc. 2004;19(3):280-6.

 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license