INTRODUCTION
Physical activity is an important factor in primary and secondary prevention, as well as in the treatment of several cardiovascular diseases [1]. Physical inactivity has been considered an important risk factor for cardiovascular diseases [2]. Studies have shown that patients with heart diseases who are enrolled in a regular exercise program and are taught about the control of the risk factors for cardiovascular diseases present both lower number of postoperative events and readmissions to hospital, besides a reduction of mortality [3, 4].
In the 1940s, the first questionings about the recommended conduct of prolonged bed rest in the management of patients with cardiovascular disease have aroused. Along with the outcomes obtained from the researches about the benefits of physical activity for the cardiovascular system, there has been a change regarding the physical activity in the treatment of cardiopath patients [5].
In 1953, Morris et al. carried out one of the first studies comparing the prevalence of the coronary artery disease (CAD) among physically active and sedentary people. They have verified the cardiovascular mortality rate among bus drivers and bus collectors. They have concluded that the physically active bus collectors presented an occurrence 30% lower among all manifestations associated to coronary disease, a 50%-lower rate of acute myocardial infarction, and an all-cause mortality rates lower than one-half of the frequency found among the bus drivers. Among the features suggested by the study, it appears that there is no need to exercise intensively or excessively to achieve some degree of protection against coronary artery disease. They have yet verified that the protection acquired though an active life-style seems to be transient, unless the activity is to be done lifelong [1,5].
In 1962, a 16-week exercise program was developed by Kellerman in Washington. It was the first physical exercise program addressed to infarcted patients and those requiring valvar surgery. This study has become the cornerstone for the development of cardiac rehabilitation programs [5].
In 1986, Shephard performed a comprehensive review of theses observational studies related to physical activity and cardiovascular diseases. The great majority has revealed a lower rate of CAD and all-cause mortality being age-specific in the more active groups. In the majority of the cases, a 2 to 3-fold increased risk associated with a sedentary lifestyle was reported. These findings were updated by a review carried out by Powell et al. in 1987. They stated that there is evidence that physical activity is inversely and casually associated to the incidence of coronary disease [1].
Over the last decades, physical activity has been incorporated as a therapeutic conduct in the management of the patient with cardiopathy associated with drug therapy and lifestyle changes, including dietary and behavioral modifications [4, 6]. A recent meta-analysis has just confirmed the beneficial effect of cardiac rehabilitation independent of coronary heart disease diagnosis, type of cardiac rehabilitation, and dose of exercise intervention. was confirmed. It was also emphasized that exercise-based programs reduce both cardiac mortality and all-cause mortality. Therefore, the true mechanism by which the exercise-based therapy improves the morbidity and mortality rates in cardiovascular disease patients still remains to be completely understood [3,4,6].
Since physical activity presents so many health benefits, it is reasonable to assume that physical activity can also become a protection factor to the patients eligible to coronary artery bypass graft (CABG) and not only as part of a rehabilitation program post-CABG. This study aims to evaluate the influence of the physical activity in the prognosis of patients who underwent CABG and the changes on frequency and intensity of physical activity of post-CABG patients.
METHODS
Study design
In a series of cases all patients who underwent CABG in a reference cardiologic hospital from August to September 2005 and in condition to answer a structured questionnaire were invited to participate in the study. The research project was approved by the Research and Ethics Committee of the Instituto de Cardiologia do Rio Grande do Sul/ Fundação Universitária de Cardiologia, and a Written Informed Consent was obtained from all participants
Characteristics of the study sample
The patients have been contacted by phone 1-year post-CABG. Those who have agreed to participate in the study have answered a structured questionnaire composed of the demographic characteristics, habits related to physical activity pre- and post-CABG, and regarding the clinical episodes post-CABG. Additional information about type of cardiac surgery, hospital length of stay, and outcome after CABG were also obtained through review of the patients' medical records.
Study variables
The following anthropometric variables were considered: gender, age, and body mass index. The patients' degree of schooling was characterized as elementary, secondary, higher education, and illiterate. The hospital length of stay, episodes and types of complications in the postoperative period, and readmissions due to cardiovascular events, all causes of cardiac reoperations, or performance of percutaneous transluminal coronary angioplasty were recorded.
Physical activity was evaluated through a recordatory questionnaire of the 12 months prior to surgery [7], the level of intensity was classified through the energy expenditure expressed in metabolic equivalents (METs), according to the model proposed by Pate et al. [8]:
Group 1: (sedentary): Those who were sedentary or were engaged in light physical activity < 3 METs;
Group 2: (moderate physical activity): Those who were engaged in physical activity for at least 30 minutes, twice a week with an energy expenditure of 3 to 6 METs
Group 3: (physically active ): Those who were engaged in physical active for more than 30 minutes, three times a week with an energy expenditure > 6 METs.
Statistical analysis
To evaluate the possible relationship between the study variables, the groups were dichotomized regarding the physical activity: sedentary (group 1) and actives (groups 2 and 3). The data were analyzed with the Statistical Package for Social Sciences software (SPSS) version 10.0 (SPSS, Chicago, IL, USA). The continuous variables were assessed by Kolmogorov-Smirnov test to analyze the normality hypotheses in order to define whether to use a parametric or nonparametric test. For all statistical tests, we considered a P value of 0.05 as significant.
RESULTS
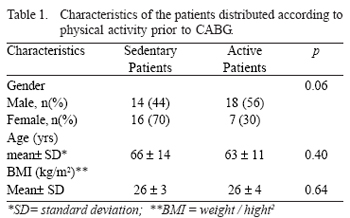
Sixty three patients underwent CABG, of these, 8 died 1-year post-CABG. The characteristics of all the 55 patients who agreed to participate in the study distributed by physical activity frequency are shown in Table 1. As for the schooling level, 27 patients (49%) have attended elementary school; 19 (35%) high-school; 5 (9%) college; and 4 patients (7%) were illiterate. Fifty patients (91%) underwent CABG alone and 5 (9%) had another associated procedure, such as plasty or valvar prosthesis.
The complications observed in the postoperative period were atrial fibrillation, readmission due to any other causes, new CABG, or performance of percutaneous transluminal coronary angioplasty, myocardial infarction, or any other. Of the 55 CABG patients, 25 (45%) developed complications. Complications occurred in patients who were both engaged in physical activity and sedentary (8 (31%) versus 17 (59%), respectively; p=0.04).
The mean hospital length of stay was 15±8 days for sedentary patients, and 12±5 days for patients engaged in physical activity prior to CABG. The median hospital length of stay was different in both groups, showing an advantage towards the patients active group (p<0.03) - Figure 1.

Fig. 1 - Hospital length of stay after CABG according to physical activity engagement prior to CABG. The mean hospital length of stay was 15 ± 8 days in sedentary patient group and 12 ± 5 days in the active patient group prior to CABG. There have been a significant difference (p<0.03) between both groups. Figure 1 shows the median hospital length of stay in both sedentary patient group and active patient group, respectively day 9 (8-15) and day 12 (9-19).
Patients who underwent CABG presented a favorable change in postoperative physical activity. After 1-year post-CABG, 33 (60%) patients were active, favorably comparing to the 25 (45%) patients who were active preoperatively. Fourteen sedentary patients (47%) became to be active (p=0.03). Walking was most reported physical activity, being performed 5 to 7 days per week for more than 30 minutes. It was reported by 17 (68%) patients preoperatively and 27 (87.9%) postoperatively.
DISCUSSION
The current study have shown a benefit from preoperative physical activity in patients who underwent CABG which favorable influenced the surgical prognosis. Concomitantly, a cardiac surgery positive effect was observed promoting a healthy lifestyle related to physical activity, which become much more frequent post-CABG.
The better performance of the active patients' group pos-CABG was characterized by both lower hospital length of stay and number of postoperative complications. The limited physical activity prior to surgery, often imposed by the restraining disease symptoms, and following surgery by the postoperative status, favors the occurrence of postoperative thromboembolic and pulmonary complications [9].
Evidences of positive physiologic changes promoted by physical activity in patients with coronary artery disease can also favorably participate in the patients' recovery post-CABG. Physical activity increases patients' functional capacity, reduces the myocardial oxygen consumption, reduces systolic and diastolic pressures, and changes favorably the lipid and carbohydrate metabolism [10,11]. Also, physical activity increases both physical performance and angina threshold in symptomatic patients with CAD, and improves myocardial perfusion [12]. In cardiac rehabilitation of patients with CAD, the myocardial perfusion improvement has been attributed to exercise training-mediated correction of coronary endothelial dysfunction. Regular physical activity restores the balance between NO production and NO inactivation by reactive oxygen species in CAD, thereby enhancing the vasodilatory capacity in different vascular beds. Endothelial dysfunction has been identified as a predictor of cardiovascular events. The partial reversal of endothelial dysfunction might be the most likely mechanism responsible for the exercise training-induced reduction in cardiovascular morbidity and mortality in patients with CAD [13].
Recently, the impact of exercise training in coronary vasomotion has been prospectively evaluated in patients with CAD. These patients have been randomized and assigned either to exercising training on a bicycle ergometer or to an inactive control group. The patiernts of both groups were characterized by the similar endothelial dysfunction degree. The mean blood flow velocity was measured by Doppler velocimetry, and the diameter of the vessel was measured by quantitative coronary angiography. The data have shown that four weeks of exercise training have partially reversed endothelial dysfunction in coronary conduit vessels of patients with CAD. The relationship strength between the mean blood flow velocity and the daily exercise training duration has suggested that the improvement in the endothelial function is strictly related to the energy expenditure during physical activity [14].
Several authors have demonstrated not only specific changes in muscular, cardiovascular, and neurohumoral systems leading to an improvement of the functional capacity, but also to a reduction in the ischemic response for submaximum work after exercising [15]. Ornish et al. [16] evaluated the effect on lifestyle changes which included 3 hours of exercise training per week in a certain degree of coronary artery stenosis. The multifactorial intervention has induced coronary stenosis regression by 3.1%, what was followed by a reduction in the cardiovascular events. In contrast, the coronary stenosis in the control group patients who received the usual care, showed a progression of 11.8%. In another study comprising 113 individuals with CAD, which have been randomized and assigned to bifactorial intervention consisting of low-fat diet and exercise training, and control groups, Schuler et al. [17] showed that the proposed program effectively prevented the coronary atherosclerosis progression, while in the control group a 0.13-mm loss in the lumen in the target region was verified after 1-year follow-up.
Physical activity has also been implied in CABG cost-effectiveness. Studies have demonstrated a mean reduction of 40% in hospital charges in those groups performing preoperative interventions, such as lifestyle changes educational programs and social support and the difference of hospital stay is, in average, less than 2 days in the active group [18, 20]. It was also observed a lower readmission risk in the active patient group [10, 11].
The CABG favorably influences promoting increased physical activity in patients who underwent surgery observed in this study was an expected finding. In our hospital facility, a daily regular routine physical activity for at least 30 minutes in the management of post-CABG patients has systematically been recommended both written and verbally. This recommendation is in accordance with the current guidelines that preconize the engagement in moderate physical activities (3-6 METs) for at least 30 minutes every day [21, 22]. However, despite our recommendations, it also known that the lifestyle changes are difficulty and remain a major challenge [23]. Therefore, other motivating factors may have participated. The awareness of the patients regarding the disease status and the treatment perspectives promoted in hospital treatment may have participated. In contrast, one of the reasons of the not-adherence to either formal rehabilitation programs or counseling to promote lifestyle changes is that after pharmacological and surgical treatment some patients feel relatively good could not realize the need to change his/her usual lifestyle [24]. This surgery favorable influence in the physical activity promotion was also observed in another study in which an increase from 16% to 47% in regular physical activity after CABG was noted [3].
CONCLUSION
Regular physical activity in the preoperative phase of CABG influences favorably the CABG patients' prognosis, reducing hospital length of stay and complications 1 year post-CABG. Concomitantly, the surgical experience promotes a lifestyle change increasing the frequency of physical activity.
REFERENCES
1. Polock MJ, Wilmark JH. Exercícios na saúde e na doença. 2ª ed. Rio de Janeiro:Medsi;1993.
2. Diário Oficial da União. Portaria nº 1893 de 15/10/2001. Criação do programa de prevenção com atividade física. Brasília;2001.
3. Charlson ME, Isom OW. Care after coronary-artery bypass surgery. N Engl Med. 2003;348(15):1456-63
4. Hedbäck B, Perk J, Hörnblad M, Ohlsson U. Cardiac rehabilitation after coronary artery bypass surgery: 10-years results on mortality, morbidity and readmissions to hospital. J Cardiovasc Risk. 2001;8(3):153-8. [
MedLine]
5. Silva E, Catai AM. Fisioterapia cardiovascular na fase tardiafase III da reabilitação cardiovascular. In: Regenga MM, ed. Fisioterapia em cardiologia: da UTI à reabilitação. 1ª ed. São Paulo:Roca;2000. p.261-310.
6. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682-92. [
MedLine]
7. Taylor HL, Jacobs DR, Schucker JK, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chron Dis. 1978; 31:741-55.
8. Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health: a recommendation from the Center for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402-7.
9. Skinner JS. Prova de esforço e prescrição de exercício para casos específicos: bases teóricas e aplicações clínicas. Rio de Janeiro:Revinter;1991.
10. Paffenbarger RS Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328(8):538-45. [
MedLine]
11. Balady GJ, Fletcher BJ, Froelicher ES. Cardiac rehabilitation programs. A statement for healthcare professional from the American Heart Association. Circulation. 1990;82:1602-10.
12. Gielen S, Schuler G, Hambrecht R. Exercise training in coronary artery disease and coronary vasomotion. Circulation. 2001;103( 1):e1-e6. [
MedLine]
13. Linke A, Erbs S, Hambrecht R. Exercise and coronary circulation: alterations and adaptations in coronary artery disease. Prog Cardiovasc Dis. 2006;48(4):270-84. [
MedLine]
14. Hambrecht R, Wolf A, Gielen S, Linke A, Hofer J, Erbs S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342(7):454-60. [
MedLine]
15. Belardinelli R, Paolini I, Cianci G, Piva R, Georgiou D, Purcaro A. Exercise training intervention after coronary angioplasty: the ETICA trial. J Am Coll Cardiol. 2001;37(7):1891-900. [
MedLine]
16. Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129-33. [
MedLine]
17. Schuler G, Hambrecht R, Schlierf G, Niebauer J, Hauer K, Neumann J, et al. Regular physical exercise and low-fat diet: effects on progression of coronary artery disease. Circulation. 1992;86(1):1-11. [
MedLine]
18. Dietl CA, Berkheimer MD, Woods EL, Gilbert CL, Pharr WF, Benoit CH. Efficacy and cost-effectiveness of preoperative IABP in patients with ejection fraction of 0.25 or less. Ann Thorac Surg. 1996;62(2):401-9.
19. Vanhees L, Schepers D, Fagard R. Comparison of maximum versus submaximum exercise testing in providing prognostic information after acute myocardial infarction and/or coronary artery bypass grafting. Am J Cardiol. 1997;80(3):257-62. [
MedLine]
20. Moller AM, Pedersen T, Villlebro N, Norgaard P. Impact of lifestyle on perioperative smoking cessation and postoperative complication rate. Prev Med. 2003;36(6):704-9. [
MedLine]
21. Bock BC, Carmona-Barros RE, Esler JL, Tilkemeier PL. Program participation and physical activity maintenance after cardiac rehabilitation. Behav Modif. 2003;27(1):37-53. [
MedLine]
22. Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB, Hademenos G, et al. Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation. 2001;103(1):163-82. [
MedLine]
23. Condon C, McCarthy G. Lifestyle changes following acute myocardial infarction: patients perspectives. Eur J Cardiovasc Nurs. 2005;5(1):37-44. [
MedLine]
24. Aldana SG, Whitmer WR, Greenlaw R, Avins AL, Salberg A, Barnhurst M, et al. Cardiovascular risk reductions associated with aggressive lifestyle modification and cardiac rehabilitation. Heart Lung. 2003;32(6):374-82. [
MedLine]

 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license