INTRODUCTION
The off-pump myocardial revascularization was initially performed by Kolessob [1] in 1967, who described his experience using the internal mammary artery in anastomosis to the anterior descending artery in six patients. Ankney [2], was the first to show a great serie of procedures, describing 200 surgeries performed without cardiopulmonary bypass (CPB) to the right coronary arteries and the anterior descending branch of the left coronary artery. He concluded that altough apparently more difficult to be performed, the anastomosis with the heart beating could present more benefits. After, Buffolo et al.[3] and Benetti et al. [4] followed him and, since then, the techinique has been praised as the first choice in the high-risk patients [5,6].
It is known that elderly are high-risk patients due the fact that they are patients with a great number of comorbities, so, because of this, some authors have dedicated to study them as a special group [7-10]. Buffolo et al. [7] mention that the myocardial revascularization surgery in patients older than 70 years is associated to a greater incidence of morbity and mortality, compared to the surgery performed in younger patients. Iglesias et al [10] analyzed the postoperative complications observed after off-pump myocardial revascularization surgey in patients older than 70 years.
In the Santa Casa of São Paulo, the off-pump myocardial revascularization with the use of intracoronary shunt was initiated with Rivetti and Gandra [11] in 1984.
Herein, we study patients with 70 years old or more who underwent myocardial revascularization by this technique aiming to analyse the preoperative characteristics, the in-hospital postoperative evolution, greater complications and mortality in this age-group.
METHODS
All data that concerned patients undergone off-pump surgery were analysed by records survey in the period from July 1989 to December 1990. From January 2000 to July 2005, a database was created totalizing 87 patients, 54 men and 33 women, among 70 and 92 years of age, with mean of 74±4.36 years. The study was approved by Clinical Research Ethics Committee of the Faculty of Medical Sciences of Santa Casa - São Paulo, filed under number 516/07. The patients were simultaneously operated without cardiopulmonary bypass by median sternotomy, being initially performed the aorta-saphenous vein proximal anastomosis under lateral clamping, following the distal anastomosis with the use of intracoronary shunt in all cases.
After surgery, the electrolytic alterations and the occurred complications were analyzed as follows: pulmonary, neurological, renal, infectious; as well as arrhythmias, perioperative infarction, congestive heart failure, necessity of blood transfusion, intubation time, stay in hospital and in intensive care unit. The hospital mortality was considered during all postoperative period.
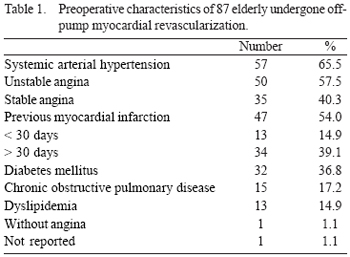
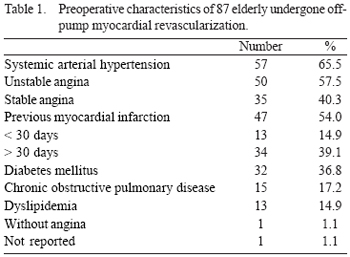
The hemodynamic study verified that the ejection fraction (EF) ranged from 20% to 76%, with mean of 55.63 ± 13.79%, being 12 patients with EF < 40%. In all group, 80 (92.0%) patients presented lesion in the anterior interventricular branch, associated or not to lesions in the right and diagonal coronary arteries. In the studied group, the patients did not have lesions in the marginal branches of the circumflex artery or in the marginal branches non-susceptible to revascularization. The considered exclusion factor for off-pump surgery was the patients who presented - through cineangiocoronariography - lesions in important marginal arteries of the circumflex artery with difficult access. The preoperative characteristics of the 87 elderly who were operated are demonstrated in Table 1.
The surgery was performed emergently in ten (11.5%) patients: three of them were operated due to an acute myocardial infarction (AMI); six, unsuccessfully post-angioplasty and one patient with postresuscitation through ventricular fibrillation. Urgently, 21 (24.1%) patients were operated and 56 (64.4%) were electively operated.
The data analysis was performed by Statistical Package for Social Sciencesversion 11.0, what consisted of absolute and relative frequency calculation, dispersion and central tendencies measurements. Records data were compared to those prospectively obtained for each variable aiming to verify the sample similarity.
RESULTS
Revascularization was performed using a graft in 44 (50.6%) patients, two grafts in 41 (47.1%) and three grafts in two patients (2.3%). The used grafts were the left internal thoracic artery, the radial artery and the greater saphenous vein. The revascularization was complete in 59 (67.8) patients.
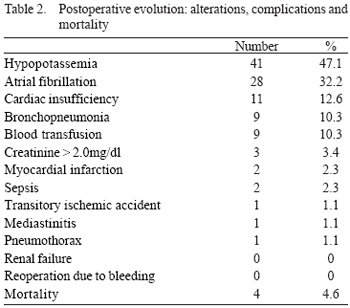
The postoperative alterations and complications are showed in Table 2. The mortality in in-hospital period was four (4,6) patients (two of them (2,3%) due to septicemia; one patient was emergently operated due to AMI who evoluted with septic shock and died in 16th day, and one patient with dyalitic chronic renal failure presented bronchopneumonia and septicemia, dying in the 10th day. One (1,1%) patient needed to a tracheostomy due to prolonged time of intubation, evoluting with mediastinitis and dying in the 73rd postoperative day. One (1.1%) patient presented spontaneous pneumothorax 48 hours after surgery evoluting to a cardiac arrest non-responsive to resuscitation maneuvers. Among four patients, three had already undergone complete revascularization and one undergone incomplete revascularization.
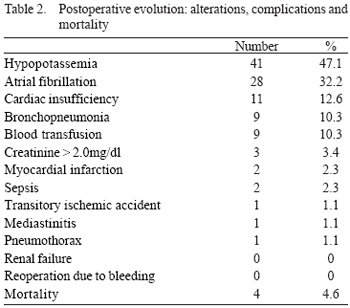
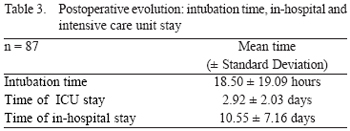
In this group, any patient was not extubated in operating room. The intubation time was from 2 to 120 hours, with mean of 18.50±19.09 hours. The ICU stay was from 24 to 360 hours, with mean of 70 hours (2.92±2.03 days) and the hospital stay was from 2 to 48 days, with mean of 10.55±7.16 days (Table 3).
DISCUSSION
We evaluated and described our experience in this group of patients above 70 year of age who underwent off-pump myocaridal revascularization and with the use of intracoronary shunt, observing the characteristics of this age-group in the preoperative and the postoperative manifestations.
The elderly with coronary artery disease presented great prevalence of AMI prior to surgery [7,10]. The low cardiac output in the postoperative of elderly who underwent off-and on-pump surgery have significant differences, as described by Al-Ruzzeh et al. [9], who report the use of intra-aortic balloon in 12% of elderly who underwent on-pump surgery versus 2% in those who underwent off-pump surgery, whilst Iglesias et al. [10] described low cardiac output in 12% of those who underwent on-pump surgery and 0% in the off-pump group. We observed that 47 (54.0%) patients of our group suffered previous AMI, inducing to a ventricular commitment and EF alterations. In this studied group, the use of intra-aortic balloon was not needed at any moment. None patient had low cardiac output as cause of death. The hemodynamic alterations were controlled only with vasoactive drugs. In our opinion, the patients with low EF presented better evolution when treated with off-pump surgery with continuous heart beating, according to experience of Buffolo et. al. [6]. Dewey et al. [12] evaluated the behavior of two groups with the same EF (25 ±4.9% and 26 ±4.2%) which the patients underwent on- and off-pump surgery, obtaining the following informations: use of intra-aortic balloon (1% and 7.7%), stroke (0.5% and 2.1%), acute renal failure (4.4% and 8.3%) and mortality (2.9% and 6.3%).
Panesar et al. [13] performed meta-analysis of 14 studies with 4,921 elderly patients undegone myocardial revascularization between 1999 and 2005, comparing the outcomes of on- and off-pump surgeries, concluding that the evolution is better in off-pump surgery concerning to mortality, stroke and less hospital stay. In our study, we achieved the same results.
When the surgical treatment occurs urgently and emergently, as Stamou et al. [14] demonstrated, it presents greater morbidity and mortality, regardless of the use or not of CPB. They described also that in the off-pump group there is less hospital stay, less incidence of renal failure, less need of intra-aortic balloon and reoperation due to bleeding. In our casuistic we performed 64.4% elective surgeries, 24.1% urgency and 11.5% emmergency surgeries, what increases the risk score of the studied group. However, we had only one death in emmergency and three in the elective surgeries. Facing the clinical characteristics of our patients (due the fact that in 35.6% of the cases the surgery was not elective with three due to AMI), we obtained satisfactory results. Analysing the perioperative AMI in the myocardial revascularization surgeries, we verified that Demers et al. [8] describe 5.1% of post-CPB and 2.0% off-pump AMI, respectively. Buffolo et. al. [7] presented result of 1.9% and 1.6% and Lima et al. [15] describe 8.0% and 4.3%, respectively. We believe that the use of intracoronary shunt promotes a better myocardial protection, avoiding ischemia of the affected region. This fact was studied in our context by Gandra and Rivetti [16] and, after by Sepic et al. [17], who concluded that the intraluminal coronary shunt is able to preserve the myocardial perfusion avoiding regional ischemia and the involvement of myocardial function. The perioperative infarction in off-pump surgery was studied by Ross [18] who compared patients undergone surgery with shunt and garroting. He reported the occurrence of perioperative myocardial infarction in 1.6% adn 4.4%, respectively, beyond to describe less hemodynamic instability in the cases in which the shunt was used. He also analyzed two groups of patients older than 80 years who underwent elective on- and off-pump surgeries with the following results: mortality (4.7% x 0%), stroke (7.1% x 0%), blood transfusion (70.4 x 33%) and time of hospital stay (11.5 x 6.3 days).
Weerasinghe et al. [19] describe that the renal function may be better preserved with off-pump surgery, specially in elderlies who present oftentimes, creatinine alteration, systemic arterial hypertension, Diabetes mellitus and EF alterations in the preoperative. Several authors describe less alteration of the renal function without use of CPB [7,20]. In our group, only three (3.4%) patients presented creatinine increase in the postoperative with values above 2.0mg/dl. Dialysis was not needed in any patient, except one who had beloged to dialysis program in the preoperative.
Demaria et al. [21] analysed patients older than 80 years of age with similar EF who underwent on- and off-pump surgeries in two groups and described that the rate of stroke was 6.3% and 0% respectively. Several authors [7,10,13,22] describe greater percentages of stroke with the use of CPB. D'Afonso et al. [23] report 12% of post-CPB mental confusion and 2.8% without use of CPB. In our study was observed one (1.1%) transitory ischemic accident and no occurrence of stroke.
Concerning to the use of hemoderivatives, there is a consensus that in off-pump surgeries its use is lesser [7,22,24,25]. Connoly [24], analyzing results of several authors, relates that the off-pump revascularization surgery presents significant decrease of occurrence of reoperation (due to bleeding) and need of perioperative transfusions when compared to the on-pump surgery. Angelini et al. [25], in randomized study, relates that there was highly significant difference regarding to need of transfusions with 45% in the on-pump group and 13% in off-pump group. In our casuistic, nine (10.3%) patients received concentrated red blood in the postoperative period for hematocrit correction and no patient needed re-exploration due to bleeding.
The infections occurred in the in-hospital period were responsable for the majority of patients' deaths of our study. According to Connolly [24], the infections of sternal incision occurs in equal incidence in on- and off-pump surgeries. In the other hand, Angelini et al. [25] report the incidence of 12% lesser of mediastinum infections in off-pump surgery. The pulmonary infections are more frequent in elderly patients,corresponding to 53% of all infections occurred in study performed by Iglesias et al. [20], in 361 elderlies on-pump revascularized. We have been observing that the elderly present more difficulty to be extubated due to current reasons such as: muscle mass decrease and more incidence of prior pulmonary diseases (embolies, pneumonia, pulmonary atelectasis and chronic obstructive pulmonary disease (COPD). The mean time of intubation was long in these patients what predisposed to pulmonary infections found in nine (10.3%) patients of our study.
The in-hospital stay has proved to be lesser when off-pump surgeries are performed [14,22,24]. In the elderly patients, there is reference of 14 days in the on-pump group and 9 days in the off-pump group [15]. The mean time of in-hospital stay in this study was 10.55±7.16 days, proving to be satisfactory for elderly patients undergone urgency and emmergency operation.
The elderly operated using CPB present mortality rate described between 9.1% and 14.6% [15,20,23]. The mortality occurred in our group was 4.6% and was mostly related to pulmonary and mediastinum infections.
CONCLUSION
Considering the morbidity and mortality rate in patients older than 70 years reported in the current literature and analysing the in-hospital behavior of our patients who underwent off-pump myocardial revascularization with the use intracoronary shunt, we can affirm that we obtained good results both in elective and non-elective surgeries with low percentages of postoperative and mortality complications.
REFERENCES
1. Kolessov VI. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Cardiovasc Surg. 1967;54(4):535-44.
2. Ankeney JL. To use or not use the pump oxygenator in coronary bypass operations. Ann Thorac Surg. 1975;19(1):108-9. [
MedLine]
3. Buffolo E, Andrade JC, Branco JN, Aguiar LR, Ribeiro EE, Jatene AD. Myocardial revascularization without extracorporeal circulation. Seven-year experience in 593 cases. Eur J Cardiothorac Surg. 1990;4(9):504-7.
4. Benetti FJ, Naselli G, Wood M, Geffner L. Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest. 1991;100(2):312-6. [
MedLine]
5. Al-Ruzzeh S, Nakamura K, Athanasiou T, Modine T, George S, Yacoub M, et al. Does off-pump coronary artery bypass (OPCAB) surgery improve the outcome in high-risk patients? A comparative study of 1398 high-risk patients. Eur J Cardiothorac Surg. 2003;23(1):50-5. [
MedLine]
6. Buffolo E, Branco JN, Gerola LR, Aguiar LF, Teles CA, Palma JH, et al. Off-pump myocardial revascularization: critical analysis of 23 years' experience in 3,866 patients. Ann Thorac Surg. 2006;81(1):85-9. [
MedLine]
7. Buffolo E, Summo H, Aguiar LF, Teles CA, Branco JN. Myocardial revascularization in patients 70 years of age and older without the use of extracorporeal circulation. Am J Geriatr Cardiol. 1997;6(1):7-15. [
MedLine]
8. Demers P, Cartier R. Multivessel off-pump coronary artery bypass surgery in the elderly. Eur J Cardiothorac Surg. 2001;20(5):908-12. [
MedLine]
9. Al-Ruzzeh S, George S, Yacoub M, Amrani M. The clinical outcome of off-pump coronary artery bypass surgery in the elderly patients. Eur J Cardiothorac Surg. 2001;20(6):1152-6. [
MedLine]
10. Iglézias JCR, Lourenção Jr.A, Dallan LAO, Puig LB, Oliveira SA. Myocardial revascularization in the elderly patient - with or without cardiopulmonary bypass? Rev Bras Cir Cardiovasc. 2003;18(4):321-5.
11. Rivetti LA, Gandra SM. Initial experience using an intraluminal shunt during revascularization of the beating heart. Ann Thorac Surg. 1997;63(6):1742-7. [
MedLine]
12. Dewey TM, Herbert MA, Prince SL, Magee MJ, Edgerton JR, Trachiotis G, et al. Avoidance of cardiopulmonary bypass improves early survival in multivessel coronary artery bypass patients with poor ventricular function. Heart Surg Forum. 2004;7(1):45-50. [
MedLine]
13. Panesar SS, Athanasiou T, Nair S, Rao C, Jones C, Nicolaou M, et al. Early outcomes in the elderly: a meta-analysis of 4921 patients undergoing coronary artery bypass grafting: comparison between off-pump and on-pump techniques. Heart. 2006;92(12):1808-16. [
MedLine]
14. Stamou SC, Hill PC, Haile E, Prince S, Mack MJ, Corso PJ. Clinical outcomes of nonelective coronary revascularization with and without cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2006;131(1):28-33. [
MedLine]
15. Lima R, Diniz R, Césio A, Vasconcelos F, Gesteira M, Menezes A, et al. Revascularização miocárdica em pacientes octogenários: estudo retrospectivo e comparativo entre pacientes operados com e sem circulação extracorpórea. Rev Bras Cir Cardiovasc. 2005;20(1):8-13.
16. Gandra SMA, Rivetti LA. Experimental evidence of regional myocardial ischemia during beating heart coronary bypass: prevention with temporary intraluminal shunts. Heart Surg Forum. 2002;6(1):10-8. [
MedLine]
17. Sepic J, Wee JO, Soltesz EG, Laurence RG, Aklog L. Intraluminal coronary shunting preserves regional myocardial perfusion and function. Heart Surg Forum. 2003;6(6):E120-5. [
MedLine]
18. Ross DE. A novel custom-made long shunt simplifies the performance and improves the results of beating-heart surgery. Heart Surg Forum. 2003;6(6):E191-3. [
MedLine]
19. Weerasinghe A, Athanasiou T, Al-Ruzzeh S, Casula R, Tekkis PP, Amrani M, et al. Functional renal outcome in on-pump and off-pump coronary revascularization: a propensity-based analysis. Ann Thorac Surg. 2005;79(5):1577-83. [
MedLine]
20. Iglesias JCR, Oliveira Jr JL, Dallan LAO, Lourenção Jr A, Stolf NAG. Preditores de mortalidade hospitalar no paciente idoso portador de doença arterial coronária. Rev Bras Cir Cardiovasc. 2001;16(2):94-104.
21. Demaria RG, Carrier M, Fortier S, Martineau R, Fortier A, Cartier R, et al. Reduced mortality and strokes with off-pump coronary artery bypass grafting surgery in octogenarians. Circulation. 2002;106(12 Suppl 1):I5-10. [
MedLine]
22. Hoff SJ, Ball SK, Coltharp WH, Glassford DM Jr, Lea JW 4th, Petracek MR. Coronary artery bypass in patients 80 years and over: is off-pump the operation of choice? Ann Thorac Surg. 2002;74(4):S1340-3. [
MedLine]
23. D'Alfonso A, Mariani MA, Amerini A, Codecasa R, Bellieni L, Proietti A, et al. Off-pump coronary surgery improves in-hospital and early outcomes in octogenarians. Ital Heart J. 2004;5(3):197-204. [
MedLine]
24. Connolly MW. Current results of off-pump coronary artery bypass surgery. Semin Thorac Cardiovasc Surg. 2003;15(1):45-51. [
MedLine]
25. Angelini GD, Taylor FC, Reeves BC, Ascione R. Early and midterm outcomes after off-pump and on-pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet. 2002;359(9313):1194-9. [
MedLine]
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license