INTRODUCTION
Some relatively recent procedure techniques, such as heart and lung transplants, are already well established [1-5].
However, circumstantial conditions may contribute to a renewed interest in anatomical aspects that, although previously studied, result in new perspectives today. One of these circumstances is the need to optimize the organs harvesting for transplant from a single donor due to the donors shortage [6.7]. Additionally, there is currently a strong tendency to perform double or bilateral lung transplants, even in cases where unilateral transplants were recommended in the past because of their better functional results in the short-term and the midterm.
The left atrium is one of the factors mentioned in the literature that limits the harvesting of a cardiac graft and two lung grafts from a single donor. This occurs because surgical techniques for lung implants in recipients recommend that venous anastomosis of the lung grafts should be performed using sutures in the atrial segment that covers the two pulmonary veins. This requires that each of the lung grafts be harvested from the donor with an atrial segment around the pulmonary vein. Therefore, the donor's left atrium must be "divided" between the two lung grafts and the cardiac graft. This could make the harvesting of three grafts from the same donor unfeasible in some situations. In this study, we propose the opening of the interatrial sulcus in order to minimize this technical difficulty.
The aim of this study is to evaluate the impact that opening the interatrial sulcus may have (in terms of gain in the area of the left atrium wall) in cases of dissection based on systemic techniques used to harvest multiple organs for heart and lung transplant.
METHODS
50 human corpses with no more than 24 hours post-mortem in the Division of Postmortem Inspection (Serviço de Verificação de Óbito - SVO) and the Institute of Legal Medicine of the Department of Forensic Science of the Secretary of Public Security of the State of Sao Paulo (IML) were studied. Corpses with macroscopically-altered hearts or with signs of previous heart surgery were excluded, as well as those who presented trauma that may have affected the heart and the great vessels.
The ages ranged from 16 to 88 years (mean = 52.3 years), and the height ranged from 155cm to 180cm (mean = 169.8cm. The weight ranged from 50kg to 90kg (mean = 67.1kg). The 50 patients included 27 male individuals, and there were 31 Caucasians and 19 non-Caucasians.
With the non fixed corpse in horizontal dorsal decubitus position, the anterior portion of the thoracic cage was removed. The sequence that was followed in the anatomical dissection complied with the correct surgical time for organs harvesting from the donor heart and lungs for heart and lung transplants, as described by Todd et al. [8].
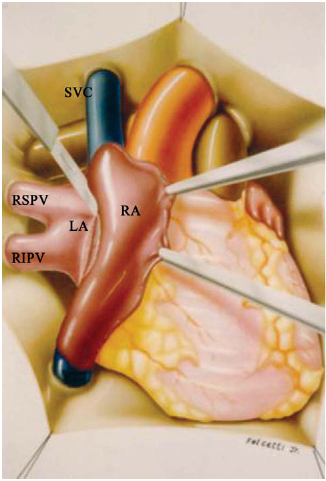
To begin, the pericardium was opened widely. The superior and intrapericardial inferior vena cavae were dissected. The aorta was dissected until surgeons reached the brachiocephalic trunk, and was then circumferentially separated from the pulmonary trunk until surgeons could identify and section the ligamentum arteriosum. The pulmonary artery trunk was isolated from the aorta. The dimension of the left atrium (from the right mediastinal side) was obtained after dissection of the interatrial sulcus (Figure 1).
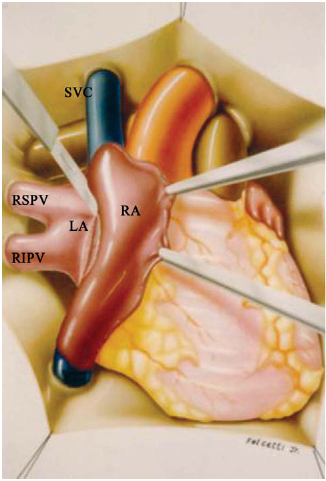
Fig. 1 - Interatrial sulcus opening
In order to obtain the atrium's measurements, the interatrial sulcus was opened longitudinally along the atrial axis, and the right atrium was tractioned and moved to the left, thus exposing a portion of the left atrial wall that had been covered by the right atrium.
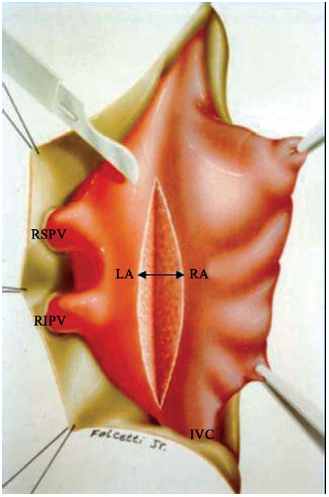
After opening the extension of the interatrial sulcus, its midpoint was identified. At this point, the dimension of the dissection margins of the atrial segment (which was exposed due to interatrial sulcus opening) was taken, and this dimension was represented as gain of left atrial wall (Figure 2).
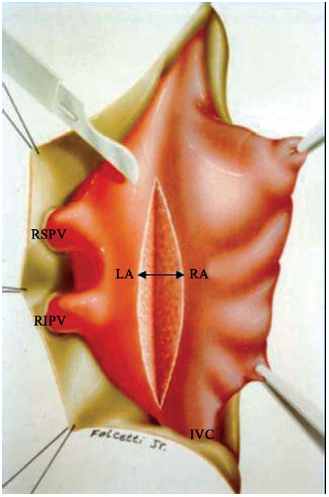
Fig 2 - Atrial wall gain after interatrial sulcus opening
Initially, all variables were descriptively analyzed by their minimum and maximum values, and the calculation of means and standard deviation. The gain of the interatrial sulcus was compared to gender, age, and ethnic variables.
Differences between groups were distinguished by Student's t-test. The level of significance for the analyses was established at 5% (p < 0.05).
The statistical calculations were performed using the SAS (Statistical Analysis System).
RESULTS
The obtained gain (which was defined by the left atrial and the calculation from the opening of the interatrial sulcus to the right) had a median value of 1.31cm, with amplitude from 0.3 to 2.5cm.
When this value was related to the gender variable, it was observed that in the 27 (54%) male cases, the gain resulting from the opening of the interatrial sulcus was 1.19 + 0.6, and in the 23 (46% ) female cases, the obtained gain was of 1.21 + 0.5cm, p=0.895.
When the value of the gain obtained with the opening of the interatrial sulcus was compared to age, it was observed that in the 24 (48%) patients under 50 years of age, the value was 1.08
+ 0.6 and, in the 26 (52%) patients at or older than 50, the gain was 1.36
+ 0.6 cm, p = 0.088.
When the results were considered in terms of ethnic groups, it was noted that the value of the gain due to sulcus opening in the 31 (62%) Caucasian cases was 1.34
+ 0.5cm and in the 19 (38%) non-Caucasian patients, the value was 1.27
+ 0,4cm with p = 0.589.
DISCUSSION
To be used for grafts in transplants, both the heart and lungs need to be harvested and appropriate portions of left atrium attached to the heart need to be preserved (as shown by Venuta et al. [9]), as do the pulmonary veins of the donor lung.
In all cases described in the literature (excluding the first isolated homologous lungs transplant in humans, performed by Hardy et al. [10], in which an individual anastomosis of the pulmonary veins was performed), the surgeons performed anastomosis, connecting the segment of the donor's left atrium containing the two homolateral pulmonary veins to the left atrium of the recepient. When reporting the harvest of the donor lung graft, different authors emphasize the importance of this technical aspect, and describe it in different ways [11-14].
However, for it to be possible to preserve an appropriate atrium segment, whether from the heart or the lungs, it is essential that, while separating the heart and lungs, the division of the left atrium be performed at the atrium's midpoint, as noted by Brodman et al. [15], on both its right and left mediastinal sides.
However, unlike the left mediastinal side of the heart, which presents a segment of atrial free wall that is located between the left pulmonary veins and the coronary sinus, the right side presents special characteristics. The anatomical structure arrangement allows the anterior recovering of the left atrium by the right atrium. Because of this superposition, the atrial walls are partially juxtaposed (by the right mediastinal side of the heart) at a point that corresponds to the limit between the right and left atria. Also, the external surface of the heart is marked by the interatrial sulcus [16-19].
As result of this anatomical arrangement, the interatrial sulcus (the limit between the left and right atria) is located very close to the confluence of the right pulmonary veins in the left atrium.
From a clinical anatomy perspective, is valuable to mention that the space to perform the incision of the left atrium by its mediastinal right side is small, allowing for a minimum acceptable margin of the left atrium around the right pulmonary veins, without the risk of crossing the interatrial sulcus and thus damaging the right atrium.
For this reason, some authors such as Cooper et al. [2] warn that the right lung harvesting (as a graft) requires excising of a portion of the interatrial septum because of the short distance between the pulmonary veins and the right atrium, which could make the simultaneous use of the heart unviable.
The Toronto Lung Transplant Group [20] and Pearson [21] also point out that, in the independent use of the heart and lungs for different recipients, it is easier to use the left lung because of the greater distance between the left pulmonary veins and the left atrial margin.
Along the same line, when Brodman et al. [15] proposed the simultaneous harvesting of heart and lung grafts from the same donor, they recommend the creation of a left atrial segment in the harvesting of the right lung through dissection of the interatrial sulcus.
Todd et al. [8] also recommended the opening of the interatrial sulcus in the donor during the simultaneous harvesting of heart and lung grafts in the cases in which a harvest of a double-lung graft is planned.
It's important to remember that, in order to perform anastomosis of the left atrium in the donor, it is necessary needed to place forceps in the atrium of the recipient that are as centered as possible on the side of the anastomosis. Cooper et al. [2] recommended that the interatrial sulcus of the receptor be dissected on the right side of the anastomosis, avoiding the clamping of the contralateral pulmonary veins.
There are conflicting opinions, such as Venuta et al. [9], that express concern about sequels in the post-implant period, which may result from cardiac manipulation. They do not recommend dissection of the interatrial sulcus and warn that such a procedure makes the use of the right lung as transplant graft unfeasable.
In the patients of this study, the obtained gain which was defined by the left atrial and the calculation from the opening of the interatrial sulcus to the right) was about 1.31cm, with amplitude of 0.3 to 2.5cm.
This result is somewhat inferior to the one described by Todd et al. [8], which was the only study in the specialized literature to approach this anatomical aspect. These authors report that the dissection of the interatrial sulcus allows us to see 1 to 3 centimeters of left atrial wall on the right side of the heart.
Authough the data indicate that there is no correlation between the gain obtained with the dissected interatrial sulcus and the gender, age and ethnic group variables, our results confirm that the opening the interatrial sulcus may provide access to a significant extension of the left atrial wall during the separation of the heart from the lungs.
REFERENCES
1. Novitzky D, Cooper DK, Barnard CN. The surgical technique of heterotopic heart transplantation. Ann Thorac Surg. 1983;36(4):476-82. [
MedLine]
2. Cooper JD, Pearson FG, Patterson GA, Todd TR, Ginsberg RJ, Goldberg M, et al. Technique of successful lung transplantation in humans. J Thorac Cardiovasc Surg. 1987;93(2):173-81. [
MedLine]
3. Patterson GA, Cooper JD, Goldman B, Weisel RD, Pearson FG, Waters PF, et al. Technique of successful clinical double-lung transplantation. Ann Thorac Surg. 1988;45(6):626-33. [
MedLine]
4. Calhoon JH, Grover FL, Gibbons WJ, Bryan CL, Levine SM, Bailey SR, et al. Single lung transplantation: alternative indications and technique. J Thorac Cardiovasc Surg. 1991;101(5):816-24.
5. Lau CL, Patterson GA. Technical considerations in lung transplantation. Chest Surg Clin N Am. 2003;13(3):463-83. [
MedLine]
6. Date H. Lung transplantation in Japan. Surg Today. 2004;34(7):565-8. [
MedLine]
7. de Perrot M, Weder W, Patterson GA, Keshavjee S. Strategies to increase limited donor resources. Eur Respir J. 2004;23(3):477-82. [
MedLine]
8. Todd TR, Goldberg M, Koshal A, Menkis A, Boychuk J, Patterson GA, et al. Separate extraction of cardiac and pulmonary grafts from a single organ donor.Ann Thorac Surg. 1988;46(3):356-9. [
MedLine]
9. Venuta F, Rendina EA, Ciriaco P, De Giacomo T, Ricci C. Separate extraction of cardiac and pulmonary grafts for left single lung transplantation. Transplant Proc. 1991;23(5):2312-4. [
MedLine]
10. Hardy JD, Webb WR, Dalton ML Jr, Walker GR Jr. Lung homotransplantation in man. JAMA. 1963;186:1065-74. [
MedLine]
11. Magovern GJ, Yates AJ. Human homotransplantation of left lung: report of a case. Ann N YAcad Sci. 1964;120:710-28.
12. Matthew H, Logan A, Woodruff MF, Heard B. Paraquat poisoning-lung transplantation. Br Med J. 1968;3(5621):759-63. [
MedLine]
13. Derom F, Barbier F, Ringoir S, Versieck J, Rolly G, Berzsenyi G, et al. Ten-month survival after lung homotransplantation in man. J Thorac Cardiovasc Surg. 1991;61(6):835-46.
14. The Toronto Lung Transplant group. Sequential bilateral lung transplantation for paraquat poisoning. A case report. J Thorac Cardiovasc Surg. 1985;89(5):734-42. [
MedLine]
15. Brodman RF, Goldsmith J, Veith FJ, Sisto DA, Bermudez R, Montefusco CM. A technique for donor lung procurement and preservation for transplantation after completion of cardiac donation. Surg Gynecol Obstet. 1988;166(4):363-6. [
MedLine]
16. Poirier P, Charpy A, Cunéo B. Abrégé d´anatomie. Paris:Masson;1908. v.2.
17. Sappey C. Traité d´anatomie descriptive. 4th ed. Paris:Adien Delahaye;1988. v.2.
18. Rouviere H. Anatomie humaine descriptive et topographique. 6th ed. Paris:Masson;1948. v.1.
19. Testut L, Latarjet A. Tratado de anatomia humana. 9ª; ed. Barcelona:Salvat;1979. v.2.
20. The Toronto Lung Transplant Group. Experience with single-lung transplantation for pulmonary fibrosis. The Toronto Lung Transplant Group. JAMA. 1988;259(15):2258-62. [
MedLine]
21. Pearson FG. Lung transplantation. Samuel Jason Mixter lecture. Arch Surg. 1989;124(5):535-8. [
MedLine]
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license