To evaluate the decrease of CPB time and its related complications in CABG using a hybrid alternative method.
Ninety patients were retrospectively analyzed between March 2000 and August 2006. All were treated with three or more grafts and divided into two groups: Group 1 was the hybrid group - 45 patients who had been operated by the hybrid technique; Group 2 was the total group - 45 patients operated in on-pump.
In the hybrid group, the CPB time varied from 20 min. to 81 min. In the total group, the CPB time varied from 60 min. to 210 min. (p<0.001). The aorta cross-clamping time varied in the first group from 7 min. to 70 min. In Group 2, from 34 to 100 min. (p<0.001). A statistically significant difference was found between these two groups in relation to the occurrence of postoperative atrium fibrillation and renal dysfunction.
Using the hybrid technique it is possible to reduce the CPB time, as well as the occurrence of some postoperative complications. Probably, this decreasing in atrial fibrillation and renal dysfunction incidences could be explained due to a less significant inflammatory activation, which is a consequence of a shorter CPB time.
Avaliar a possibilidade da redução do tempo de circulação extracorpórea (CEC) e das complicações relacionadas a esta variável na revascularização do miocárdio (RM), utilizando o método híbrido como alternativa.
Noventa pacientes foram analisados, retrospectivamente, entre março/2000 e agosto/2006. Todos foram revascularizados com três ou mais enxertos e divididos em doisgrupos: híbrido - 45 pacientes que foram operados pela técnica híbrida; total - 45 pacientes operados com CEC. Resultados: No grupo híbrido, o tempo de CEC variou de 20 a 81 minutos e, no grupo total, de 60 a 210 minutos (p<0,001). O tempo de pinçamento aórtico variou de 7 a 70 minutos no primeiro grupo e de 34 a 100 minutos (p<0,001) no segundo grupo. Foi encontrada diferença estatisticamente significativa entre os grupos em relação à incidência de fibrilação atrial e à disfunção renal.
Utilizando-se a técnica híbrida é possível reduzir o tempo de CEC e a incidência de algumas complicações pós-operatórias. Provavelmente, esta redução nas incidências de fibrilação atrial e disfunção renal podem ser explicadas por uma redução na resposta da inflamatória conseqüente a um tempo de CEC menor.
INTRODUCTION
The off-pump coronary artery bypass graft (CABG) has been widely used in the treatment of multiarterial coronary disease; however, performing myocardial revascularization surgery without CPB is sometimes not possible due to the intra-operative hemodynamic instability caused by the traction and torsion maneuvers of the heart to expose the coronary vessels during bleeding of myocardial ischemia during anastomosis [1-3].
The use of CPB and the diastolic arrest of the heart induced by cardioplegia solution favor the exposition of the epicardial vessels. They maintain appropriate hemodynamic support and control the temperature of patient. However, especially after an extended period of time time, the CPB, causes metabolic changes [4], endocrine responses [5], inflammatory responses [6], reduction of the number and function of platelets [7] and cognitive changes [8].
Cardiopulmonary bypass (CPB) also can provoke a sequence of organ dysfunctions [9] as a consequence of the inflammatory reaction caused by the contact of the blood with the non-endothelized circuit surface of the heart-lung machine.
The alternative proposed herein for treatment of patients with three-vessel disease is to initiate the CABG without CPB to perform anastomosis of the diagonal and anterior descending branches and the right coronary artery, and to use CPB for less time, only when it an ample rotation and traction of the heart is necessary for treating the posterior lateral branches of the left coronary artery.
This present study aims to evaluate the reduction of CPB and aortic clamping time using a hybrid method as alternative, and to evaluate the incidence of complications related to CPB time.
METHODS
Ninety patients referred to CABG between March 2000 and August 2006 were retrospectively analyzed. All had been treated with three or more grafts. The Hybrid Group (45 patients) was composed of all patients operated on using the hybrid technique in this period after presenting unfavorable anatomy for the off-pump CABG. The Total Group was made up of 45 patients consecutively operated on on-pump, and was used as a comparative group. The preoperative characteristics of both groups were recorded and statistically analyzed (Table 1).
The criteria used by the surgical team to define unfavorable coronary anatomy to off-pump surgery were: intramyocardial target vessels at lateral wall, marginal branches with a diameter less than 1.5 mm, or presence of hypertrophic myocardium. The Parsonnet index was used to predict the operative mortality risk (Table 2).
All patients had been operated on using a median sternotomy. In both groups, slight hypothermia (32ºC) was used during the CPB and proximal anastomosis in the aorta was completed with lateral clamping. In the hybrid group, the OCTOPUS 3 MEDTRONIC
® stabilizer was used during distal anastomosis without CPB. Hyperkalemic normothermic 4:1 blood cardioplegia was used in the Total Group and in the distal anastomosis of the Hybrid Group during on-pump.
All data was submitted to statistical evaluation and the
a-error was set at 5%. The nominal variables were analyzed using Fisher's exact test or the Chi-Square test. The continuous parametric variables were analyzed using Student's t-test and the non-parametric continuous variables with the Mann-Whitney test.
RESULTS
The groups were similar in age, gender and risk factors for coronary disease (p>0.05) (Table 1). The incidence of NYHA III/IV cardiac insufficiency was higher in the Hybrid Group (p<0.001). The mean of preoperative mortality risk estimation score (Parsonnet index) was 14.59 ± 6.27 in the Hybrid Group, and 7.6 ± 5.18 in the Total Group (p<0.001) (Table 2).
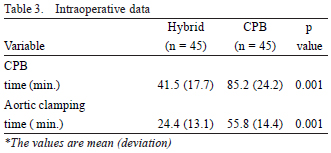
In the Hybrid Group, the CPB time was 41.5 ± 17.7 min., and in the Total Group, 85.2 ± 24.2 min (p<0.001). The aortic clamping time was 24.4 ± 13.1 min. in the first group and 55.8 ± 14.4 in the second (p<0.001) (Table 3). The mean number of grafts for each patient in the Hybrid Group was 3.31 and was 3.35 in the Total Group. The proportion of arterial grafts was 56% in the first group and 52% in the second.
Renal dysfunction, which was defined as plasmatic creatinine
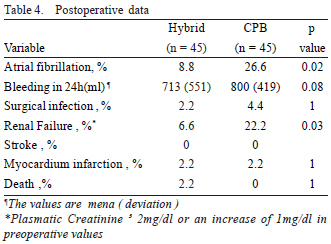
> 2mg/dl or an increase of 1mg/dl in preoperative values, was observed in 6.6% of the patients of the Hybrid Group and in 22.2% of the patients of the Total Group (p=0.03). Atrium fibrillation occurred in 4 patients from the Hybrid Group and in 12 patients from the Total Group (p=0.02). A statistically significant difference was not observed when comparing the quantity of blood collected by drains, incidence of surgical infection, trans-operative infarction, stroke and hospital mortality between the two groups (Table 4).
DISCUSSION
CPB supported the development of intracardiac surgeries and complex procedures where a clean and static field is necessary, thus allowing for great advances in cardiac surgery. However, its harmlessness is questioned because of problems related with its use, which are mainly associated with prolonged perfusion time [9-11].
Perfusion time is related to a systemic inflammatory response that leads to changes at cellular and humoral levels [12,13], such as the activation of complement system and coagulation cascade, causing alterations in vascular permeability and reactivity. Neurologic dysfunctions are related to on-pump CABG [8,14], especially with a prolonged CPB time [15]. Because of its adverse effects, alternatives that could diminish the morbidity of CPB have been investigated. The use of antifibrinolytic agents [16,17], hemofiltration [18,19] and off-pump CABG [20,21] are technological advents in this procedure. In this way, the off-pump CABG is undoubtedly a great advance; however, the application of this technique has technical and planning limitations. The cardiac manipulation to expose the coronary branches brings hemodynamic complications that can limit the procedure. Major alterations in the ventricular filling pressures have already been described [1,3].
Soltoski et al. [22] described a conversion rate of 25% in CABG procedures without CPB and suggested one selective behavor. The insistence on continuing the procedure without CPB in less-than-ideal hemodynamic conditions is not uncommon, but it should be discouraged because its serious consequences. In this study, we considered an alternative method, which may reduce morbidity from CPB in three-vessel disease.
This study showed that perfusion time, the most common factor in the development of complications after CPB, could be reduced using a hybrid method (Table 3). Aortic clamping time also presented a statistically significant reduction.
The use of CPB and perfusion time can affect the occurrence of postoperative renal dysfunction [9,23]. We have shown that the group with the shortest perfusion time was the Hybrid Group, which also presented a statically significant reduction in postoperative renal dysfunction.
A reduction in the incidence of postoperative atrial fibrillation (AF) was also found in this study when both groups were compared. It is known that incidences of atrial fibrillation are lower in the off-pump CABG series [24]. Many factors are related to postoperative atrial fibrillation. The reduction in perfusion time and most likely in inflammatory response could explain the decrease in the incidence of AF in the hybrid group.
In a 2,630-patient on-pump CABG study, Lahtinen et al. described that atrial fibrillation was a major determinant in the occurrence of postoperative strokes [25]. From these cases, the authors reported a 2% incidence of stroke and previous atrial fibrillation of 36.7%. The mortality in this neurologically damaged group was 23.1%. In our sample, there were no strokes in either group. This could be explained by the relatively small number of cases that underwent MR in our study when compared with the Lahtinens study [25]. Perhaps in another study with stronger statistical power, a difference in postoperative stroke occurrence in Hybrid Group would be found.
The number of postoperative infarcts, deaths, surgical infections and strokes, as well as the bleeding volume, were similar between the groups. These data show that it is possible and safe to reduce the CPB time without decreasing of the quality of the procedure.
CONCLUSION
The use of hybrid technique can reduce CPB and aortic clamping time in the MR of patients with multiple coronary artery diseases without compromising the quality of the procedure. Although this study presents some limitations inherent to a retrospective study, our data show that the incidences of postoperative atrial fibrillation and renal dysfunction can be reduced using the hybrid technique.
REFERENCES
1. D'Ancona G, Karamanoukian H, Lima R, Ricci M, Bergsland J, Rossman J, et al. Hemodynamic effects of elevation and stabilization of the heart during off-pump coronary surgery. J Card Surg. 2000;15(6):385-91. [
MedLine]
2. Kim KB, Lim C, Ahn H, Yang JK. Intraaortic balloon pump therapy facilitates posterior vessel off-pump coronary artery bypass grafting in high-risk patients. Ann Thorac Surg. 2001;71(6):1964-8. [
MedLine]
3. Oliveira PP, Braile DM, Vieira RW, Petrucci Junior O, Silveira Filho LM, Vilarinho KA, et al. Hemodynamic disorders related to beating heart surgery using cardiac stabilizers: experimental study. Rev Bras Cir Cardiovasc. 2007;22(4):407-15. [
MedLine]
4. Ascione R, Talpahewa S, Rajakaruna C, Reeves BC, Lovell AT, Cohen A, et al. Splanchnic organ injury during coronary surgery with or without cardiopulmonary bypass: a randomized, controlled trial. Ann Thorac Surg. 2006;81(1):97-103. [
MedLine]
5. Hoda MR, El-Achkar H, Schmitz E, Scheffold T, Vetter HO, De Simone R. Systemic stress hormone response in patients undergoing open heart surgery with or without cardiopulmonary bypass. Ann Thorac Surg. 2006;82(6):2179-86. [
MedLine]
6. Hoel TN, Videm V, Mollnes TE, Saatvedt K, Brosstad F, Fiane AE, et al. Off-pump cardiac surgery abolishes complement activation. Perfusion. 2007;22(4):251-6. [
MedLine]
7. Ballotta A, Saleh HZ, El Baghdady HW, Gomaa M, Belloli F, Kandil H, et al. Comparison of early platelet activation in patients undergoing on-pump versus off-pump coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2007;134(1):132-8. [
MedLine]
8. Chernov VI, Efimova NY, Efimova IY, Akhmedov SD, Lishmanov YB. Short-term and long-term cognitive function and cerebral perfusion in off-pump and on-pump coronary artery bypass patients. Eur J Cardiothorac Surg. 2006;29(1):74-81. [
MedLine]
9. Taniguchi FP, Souza AR, Martins AS. Tempo de circulação extracorpórea como fator risco para insuficiência renal aguda. Rev Bras Cir Cardiovasc. 2007;22(2):201-5. [
MedLine]
10. Habib RH, Zacharias A, Engoren M. Determinants of prolonged mechanical ventilation after coronary artery bypass grafting. Ann Thorac Surg. 1996;62(4):1164-71. [
MedLine]
11. Byhahn C, Strouhal U, Martens S, Mierdl S, Kessler P, Westphal K. Incidence of gastrointestinal complications in cardiopulmonary bypass patients. World J Surg. 2001;25(9):1140-4. [
MedLine]
12. Moura HV, Pomerantzeff PMA, Gomes WJ. Síndrome da resposta inflamatória sistêmica na circulação extracorpórea: papel das interleucinas. Rev Bras Cir Cardiovasc. 2001;16(4):376-87.
13. Saatvedt K, Lindberg H, Michelsen S, Pedersen T, Geiran OR. Activation of the fibrinolytic, coagulation and plasma kallikrein-kinin systems during and after open heart surgery in children. Scand J Clin Lab Invest. 1995;55(4):359-67. [
MedLine]
14. Borger MA, Peniston CM, Weisel RD, Vasiliou M, Green RE, Feindel CM. Neuropsychologic impairment after coronary bypass surgery: effect of gaseous microemboli during perfusionist interventions. J Thorac Cardiovasc Surg. 2001;121(4):743-9. [
MedLine]
15. Ridderstolpe L, Ahlgren E, Gill H, Rutberg H. Risk factor analysis of early and delayed cerebral complications after cardiac surgery. J Cardiothorac Vasc Anesth. 2002;16(3):278-85. [
MedLine]
16. Ray MJ, O'Brien MF. Comparison of epsilon aminocaproic acid and low-dose aprotinin in cardiopulmonary bypass: efficiency, safety and cost. Ann Thorac Surg. 2001;71(3):838-43. [
MedLine]
17. Jimenez JJ, Iribarren JL, Lorente L, Rodriguez JM, Hernandez D, Nassar I, et al. Tranexamic acid attenuates inflammatory response in cardiopulmonary bypass surgery through blockade of fibrinolysis: a case control study followed by a randomized double-blind controlled trial. Crit Care. 2007;11(6):R117. [
MedLine]
18. Maluf MA, Mangia C, Bertuccez J, Silva C, Catani R, Carvalho W, et al. Estudo comparativo da ultrafiltração convencional e associação de ultrafiltração convencional e modificada na correção de cardiopatias congênitas com alto risco cirúrgico. Rev Bras Cir Cardiovasc. 1999;14(3):221-36.
19. Ungerleider RM. Effects of cardiopulmonary bypass and use of modified ultrafiltration. Ann Thorac Surg. 1998;65(6 Suppl):S35-8.
20. Buffolo E, Andrade JC, Succi JE, Leão LE, Cueva C, Branco JN, et al. Revascularização direta do miocárdio sem circulação extracorpórea: descrição da técnica e resultados iniciais. Arq Bras Cardiol. 1982;38(5):365-73. [
MedLine]
21. Buffolo E, Branco JN, Gerola LR, Aguiar LF, Teles CA, Palma JH, et al. Off-pump myocardial revascularization: critical analysis of 23 years experience in 3,866 patients. Ann Thorac Surg. 2006;81(1):85-9. [
MedLine]
22. Soltoski P, Salerno T, Levinsky L, Schmid S, Hasnain S, Diesfeld T, et al. Conversion to cardiopulmonary bypass in off-pump coronary artery bypass grafting: its effect on outcome. J Card Surg. 1998;13(5):328-34. [
MedLine]
23. Massoudy P, Wagner S, Thielmann M, Herold U, Kottenberg-Assenmacher E, Marggraf G, et al. Coronary artery bypass surgery and acute kidney injury: impact of the off-pump technique.Nephrol Dial Transplant. 2008. [
MedLine]
24. Stamou SC, Pfister AJ, Dangas G, Dullum MK, Boyce SW, Bafi AS, et al. Beating heart versus conventional single-vessel reoperative coronary artery bypass. Ann Thorac Surg. 2000;69(5):1383-7. [
MedLine]
25. Lahtinen J, Biancari F, Salmela E, Mosorin M, Satta J, Rainio P, et al. Postoperative atrial fibrillation is a major cause of stroke after on-pump coronary artery bypass surgery. Ann Thorac Surg. 2004;77(4):1241-4. [
MedLine]


 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license