CLINICAL DATA
14-month-old-girl, 7.1 kg, from Ilha Solteira, São Paulo State, Brazil, was referred to our Service after being adopted by a family who did not know her medical history.
During her first physical examination, the patient was in good general health, eupneic, pale, hydrated and cyanotic ++/4+. Low weight and nutritional gain, constant episodes of cyanosis and motor deficit in the upper right limb, as a result of a previous stroke, for which she used phenobarbital.
Cardiac auscultation revealed split S2 and hyperphonesis of the second sound in the lower left sternal edge and systolic ejection murmur +++/6+ in mid-left sternal edge. Pulmonary auscultation was normal. Unchanged abdomen. Presence of peripheral pulses, strong and symmetrical. Peripheral saturation of 82% in room air.
Propranolol was introduced, the patient received additional examinations, and an operation to correct the defect was scheduled. Due to child custody issues, she didn't return for another nine months, and was in bad general condition, with fever and diarrhea. The clinical presentation and the exams suggested enterovirus and, after five days in the ward, she improved significantly, but with frequent crises of cyanosis, a fact that was associated with the child custody issues, and which triggered the recommendation of surgical correction during the same hospital stay.
ELECTROCARDIOGRAM
Sinus rhythm, heart rate of 150 bpm. SÂP 45°, SÂQRS + 120°, QTc 0.43s. Right atrial overload, spiked P-wave amplitude of 3mm at D2. Right ventricular overload with R-wave amplitude of 25mm at V1.
RADIOGRAM
Visceral
situs solitus with levocardia. Cardiac area with cardiothoracic index of 0.54, with middle arch slightly bulging and an aortic arch to the left. Normal transparency of the pleuropulmonary fields.
ECHOCARDIOGRAM
Tetralogy of Fallot (TOF) of unfavorable anatomy, with
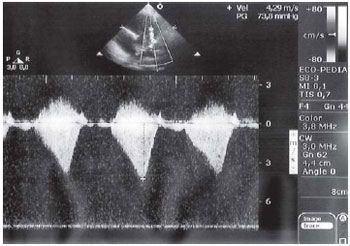
situs solitus with levocardia, venoatrial, atrioventricular and normal ventriculoarterial connections. Aortic diameter of 18mm, pulmonary valve ring, confluent right and left pulmonary arteries both at 9mm. Continuous Doppler revealed turbulent and accelerated flow with peak systolic gradient between the right ventricle (RV) and pulmonary trunk of 73.8 mmHg, revealing a large infundibular component due to the aspect of the curve with a late peak (Figure 1).
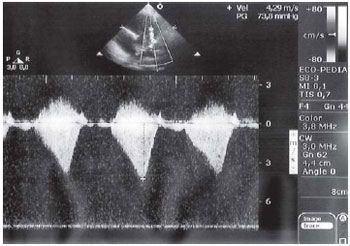
Fig. 1 - Continuous Doppler for pulmonary flow analysis obtained through parasternal short axis view showing infundibular systolic peak of 73.8 mmHg
During the first consultation, TOF was strongly considered, supported by an echocardiogram of another practice and by the patient's use of propranolol. The previous use of phenobarbital and the frequent absence seizures due to previous stroke and severe cyanosis led to our recommendation of an urgent operation. However, the child'custody situation of the patient made it difficult to treat in appropriate time, exposing her to greater surgical risk.
OPERATION
After going under anesthesia, the patient presented serious hypoxia crisis with peripheral saturation of 32%. We used an emergency median transsternal thoracotomy; we opened the pericardium, performed a purse-string suture in the aorta and vena cava, used heparinization with 4 mg/kg, introduced cannulas in the aorta and vena cava and started with the assistance of cardiopulmonary bypass with hypothermia at 28°C.
After aortic clamping, blood cardioplegia was initiated - hypothermic at 4ºC, anterograde, intermittent, with volume of 20 ml/kg at 20-minute intervals, which was administered after opening the right atrium and draining the left atrium through the interatrial septum.
Incision in anterior side of the pulmonary trunk, pulmonary valve ring and right ventricular outflow tract (RVOT) were performed. The valve ring was measured using Hegar dilator and presented 9mm; according to the body surface, it should be 11.3 mm, so it needed to be enlarged.
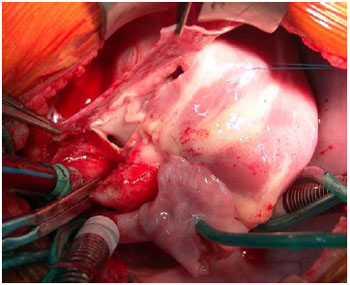
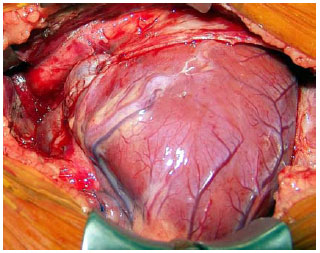
The left pericardium was carefully dissected (preserving the maximum possible number of blood vessels), and it was pediculated to the enlargement of the right components (Figure 2). The suture of the pericardium, which should be enlarged - was begun at the lateral edge and was completed by implanting the tile-shaped pediculated pericardium (Figure 3). 6-0 polidioxanone thread was used throughout the suture. The aim was to allow for growth and to avoid future calcification, among other known problems existing with several materials that can be used for this purpose [1,2].
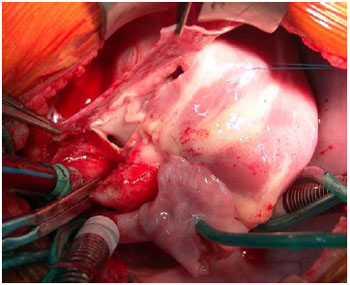
Fig. 2 - Surgical aspect of the pediculated autologous pericardium (tweezers) before enlargement. The anterior side of the right ventricular outflow tract, valve ring and pulmonary trunk can also be observed
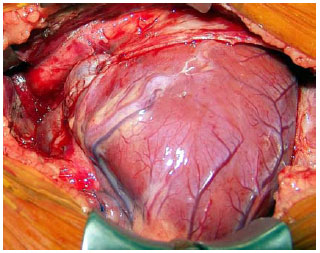
Fig. 3 - Final aspect after pediculated autologous pericardium implant enlarging the right ventricular outflow tract, valve ring and pulmonary trunk
The interventricular communication (IVC) was closed with a bovine pericardium patch with 6-0 polypropylene continuous suture through the opening in RVOT.
The infusion time was 84 minutes and myocardial ischemia lasted 56 minutes.
In the Intensive Care Unit, the patient presented excess bleeding, with a significant change in coagulogram. She was referred to the operating room for a review of hemostasis and retained clot syndrome was noticed. She presented with pneumonia and was treated with the appropriate antibiotics for 14 days.
Intrahospital controlled echocardiogram showed endocarditis, and a clinical treatment of antibiotics was chosen. The sequential examinations showed a presence of residual (2mm) interventricular communication without hemodynamic repercussions.
The patient was discharged from hospital only on the 23
rd postoperative day, more than a week later, as doctors were awaiting the decision of the Council managing the child's custody.
At one-year and seven months follow-up in our clinic, the patient presented with appropriate weight gain within normal limits for her age; she was asymptomatic, in NYHA functional class I, and the echocardiography revealed the presence of moderate-to-severe pulmonary insufficiency and normal RV global function.
REFERENCES
1. Ilbawi MN, Idriss FS, DeLeon SY, Muster AJ, Gidding SS, Berry TE, et al. Factors that exaggerate the deleterious effects of pulmonary insufficiency on the right ventricle after tetralogy repair. Surgical implications. J Thorac Cardiovasc Surg. 1987;93(1):36-44. [
MedLine]
2. Croti UA, Barbero-Marcial M, Jatene MB, Riso AA, Tanamati C, Aiello VD, et al. Classificação anatômica e correção cirúrgica da atresia pulmonar com comunicação interventricular. Rev Bras Cir Cardiovasc. 2001;16(4):321-36.
3. Silva, PR. Retalho de pericárdio pediculado vascularizado autógeno para aortoplastia e correção da coarctação simples de aorta torácica, ou associada à hipoplasia, atresia ou interrupção do arco aórtico. Rev Bras Cir Cardiovasc. 2006;21(4):453-60.
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license