Camila de Christo Dorneles0; Luiz Carlos Bodanese0; João Carlos Vieira da Costa Guaragna0; Fabrício Edler Macagnan0; Juliano Cé Coelho0; Anibal Pires Borges0; Marco Antonio Goldani0; João Batista Petracco0
DOI: 10.1590/S0102-76382011000200012
INTRODUCTION
Blood transfusion and hemocomponents are important technologies in modern therapy. If it is appropriately used in significant morbidity or mortality conditions, and when its not effectively prevented or controlled in any other way, it can save lives and improve patients' health. However, as any other therapeutic interventions, it can lead to acute or late complications, such as the risk for transmission of infectious agents, among other clinical complications [1].
Blood transfusion is related to the occurrence of a transfusion reaction, transmission of infection, increased postoperative morbidity and mortality, risk of immunosuppression and the cost of hospitalization [2-4]. Cardiac surgery is associated with high rates of blood transfusion, ranging from 40% to 90% in most studies [5-7]. Transfusions have been associated with high morbidity and mortality in patients and some recent studies have demonstrated worse outcomes, including increased occurrence of renal failure and infection, as well as respiratory, cardiac and neurological complications in transfused patients compared to those who were not transfused after cardiac surgery [7-9].
The occurrence of bleeding is a frequent complication of cardiovascular surgery [10]. Approximately one-third of the operated patients require blood transfusion, being responsible for the consumption of 10% to 25% of the hemoderivatives in the United States [10-13].
The aim of this study was to recognize the risk factors associated with blood transfusion in the postoperative period of cardiac surgery, thus, it allows strategies to be drawn to reduce these comorbidities in this group of patients.
METHODS
We conducted a retrospective cohort study using data from the Cardiovascular Surgery Department of Sao Lucas Hospital at PUCRS, from 4028 patients who underwent coronary artery bypass graft (CABG), valve replacement (VR) or combined surgeries (CABG and VR) between January 1996 and December 2009. Patients who received two or more units of red packed blood cells in the postoperative period (PO) of the surgeries. The patients received blood transfusions when there was excessive bleeding after surgery (above 400 ml in the first postoperative hours or above 100 ml / hour for the first 6 postoperative hours) requiring surgical intervention.
The pre and perioperative variables analyzed were: female gender, age over 65 years, smoking, obesity (BMI e" 30kg / m2), chronic obstructive pulmonary disease (COPD) clinically diagnosed and / or through chest X-ray and / or spirometry, and / or drug therapy (corticosteroids or bronchodilators), chronic renal failure (creatinine> 1.5 mg / dL or prior hemodialysis), active infectious process (through laboratory tests), prior cardiac surgery, history of previous diseases as diabetes (DM), systemic arterial hypertension (SAH), peripheral vascular disease (PVD), cerebrovascular accident (CVA), atrial fibrillation (AF) and acute myocardial infarction (AMI), unstable angina (UA), functional class 3 and 4 of heart failure according to criteria of the New York Heart Association (NYHA), ejection fraction below 40% (measured by echocardiography), surgical priority (emergency surgery / emergency as a single variable and defined as the need for intervention up to 48 hours due to imminent risk of death or unstable hemodynamic condition), extracorporeal circulation time over 120 minutes, use of intra-aortic balloon pump (IABP).
The postoperative variables analyzed as possible complications related to transfusion of hemoderivatives were: sepsis and respiratory infection diagnosed by isolated organisms in culture associated with fever and elevated white blood cell count; mediastinitis diagnosed from the presence of pain, warmth, redness, and pus in the wound of the sternum, presence of sternal instability and fever, as well as through a tomography of the thorax, postoperative AMI, diagnosed by the evidence of subepicardial current with the onset of Q wave, subendocardial injury current with increased markers of myocardial necrosis (troponin I above 10µg/dL and CK-MB five times higher than the reference value or above 10% of total CK) or new bundle branch block with elevation of markers, atrial fibrillation (AF) confirmed by electrocardiographic analysis, acute renal failure (ARF), with an increase of creatinine and need for dialysis, acute respiratory distress syndrome (ARDS), with chest radiograph showing alveolar-interstitial infiltrates, micro and / or macronodular, bilateral and asymmetric and an oxygenation index (PaO2/FiO2) <200 mmHg, cerebrovascular accident (CVA), diagnosed by clinical signs of neurological deficit and CT compatible; the death rate within 30 days after surgery and hospitalization time in patients receiving hemoderivatives or not were also analyzed.
The quantitative variables were described by mean and standard deviation and the categorical variables were described by means of absolute and relative frequencies. In addition to the descriptive analysis, univariate analysis was performed from the Student t test for the quantitative variables and Pearson's chi-square test and / or Fisher exact test for the categorical variables. To assess the possible intervening variables, multivariate analysis was performed by the bivariate logistic regression (stepwise forward), in which all pre-and perioperative factors were adjusted as possible confounding factor, with P <0.1 for entry logistic regression. The variables with P <0.05 were considered significant. The software SPSS (Statistical Package for the Social Sciences, version 18.0) were used for statistical analysis.
This study research project was submitted and approved by the PUCRS Research Ethics Committee.
RESULTS
In this retrospective study, 4.028 patients were included, 62.9% (n = 2,533) were male and 37.1% (n = 1,495) were female. Regarding the type of surgery, 67.2% (n = 2706) underwent CABG, 27.4% (n = 1,102) CTV and 5.6% (n = 225) underwent combined surgery (CABG + VR). Considering these patients, 22.7% (n = 916) required blood transfusion in the postoperative period of cardiac surgery. Only 139 (3.45%) patients in the study sample underwent surgery without extracorporeal circulation. In Table 1, the patients pre-and perioperative data are shown.
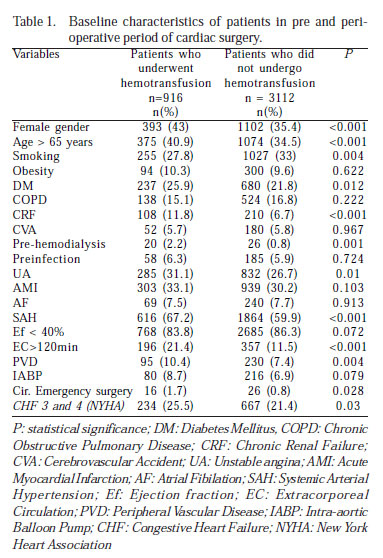
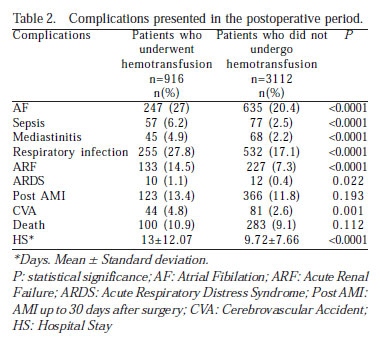
Ten postoperative complications were evaluated in relation to the use of packed red blood cells (RBC) (Table 2). Patients who received blood transfusions had significantly more infectious episodes as mediastinitis (4.9% vs. 2.2%; P = 0.001) respiratory infection (27.8% vs. 17.1%; P = 0.001), and sepsis (6.2% vs. 2.5%; P = 0.001). This group of patients also had more episodes of AF (27% vs. 20.4%; P = 0.001), ARF (14.5% vs. 7.3%; P = 0.001) and CVA (4.8% vs. 2.6%; P = 0.001). AMI and ARDS were not statistically significant, but showed a tendency. Moreover, the length of hospital stay after surgery was higher in the group that received blood transfusion (13 ± 12.07 days vs. 9.72 ± 7.66 days; P = 0.001). However, mortality did not differ between patients who received RBC as compared to those who were not transfused (10.9% vs. 9.1%; P = 0.112).
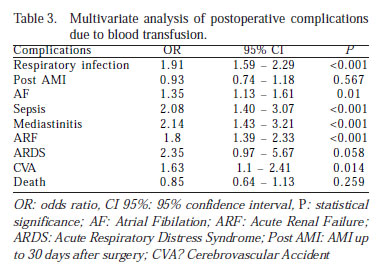
The postoperative complications were included in multivariate analysis (Table 3), and adjusted for pre-and perioperative factors mentioned above, and were related as risk factors due to blood transfusion: respiratory infection (OR: 1.91; CI95%: 1.59-2.29; P<0.001), ARDS (OR: 2.35; CI95%: 0.97-5,67; P=0.058), (NRAF (OR:1.35; CI95%: 1.13-1.61; P<0.01), sepsis (OR: 2.08; CI95%: 1.4-3.07; P<0.001), mediastinitis (OR: 2.14; CI95%: 1.43-3.21; P<0.001), CVA (OR: 1.63; CI95%: 1.1-2.41; P=0.014) and ARF (OR: 1.8; CI95%: 1.39-2.33 days; P <0.001). AMI and death rate were not statistically significant.
DISCUSSION
The study results suggest that blood transfusion in the studied sample is related to the risk of infectious events (such as mediastinitis, respiratory infection, sepsis). The transfused patients had also more episodes of AF, ARF and CVA. ARDS appears as a tendency to risk factor and can not be dismissed.
The association between packed red cells transfusion and postoperative complications (PO) for cardiac surgery is often described in the literature. In a study conducted by Koch et al. [14], when analyzing the ratio of units of packed red cells administered to adult patients and the risk of morbidity and mortality in patients undergoing CABG, it was concluded that from the 11,963 patients analyzed, 5,184 (49%) received at least one unit of RBC.
The authors also concluded that there is a relationship between each RBC unit transfused and the risk of morbimortality in the postoperative period. According to the study, each administered unit increases by 77% the postoperative mortality risk and 100% the risk of developing any renal complication, 76% the risk of developing postoperative infections, cardiac complications in 55% and 37% the risk of neurological complications. These associations remained strong even after the risk adjustment factors causing postoperative complications. The authors also reported the importance of stratifying high-risk groups for transfusion and then, modulate the pre-and perioperative interventions that help to reduce blood transfusion in the postoperative period, and, consequently, the risk of complications.
In a study conducted by Möhnle et al. [15] in patients who had low risk of developing postoperative complications of cardiac surgery, it was observed that, despite the low risk patients who received blood transfusion had an increased risk of developing cardiac events, as well as an increase in surgical site infections. However, the authors report that the study's findings related to infectious, renal complications and hospital mortality should be carefully analyzed, mainly due to the fact that the group of transfused patients differs in several characteristics from the group that did not received blood transfusions in the postoperative period.
Karkouti et al. [16] also reported that the need for blood transfusion in the postoperative period of cardiac surgeries is directly associated with complications such as sepsis, ARDS, ARF and death.
In this study, a tendency toward higher pulmonary complication rates in transfused patients was noted, reaching statistical significance for lower respiratory tract infection, but not for ARDS. The design of the study, however, did not allow to differentiate ARF due to TRALI (Transfusion-related Acute Lung Injury) from other causes such as ARDS and lower respiratory tract infection.
Specifically in relation to risk of pulmonary complications, Koch et al. [17], in another study reported that blood transfusion is associated with high risk of ARF, ARDS, need for reintubations due to pulmonary causes, long-term intubations and longer hospitalization period in the intensive care unit. The same study concludes that the use of plasma is associated with more pulmonary complications after surgery when compared to other hemoderivatives.
Another acute pulmonary complication caused by blood transfusion, known as TRALI, the receiver of hemoderivatives develops signs and symptoms of respiratory compromise due to a non-cardiogenic pulmonary edema. Evidence of hypoxemia with a ratio of PaO2/FiO2 <300, associated with bilateral pulmonary infiltrates and without fluid overload, are diagnostic criteria for TRALI. But the most common criterion for diagnosis is the temporal criterion between the transfusion and the onset of signs and symptoms. They usually occur 1 or 2 hours after the transfusion, with 100% of the patients presenting the symptoms 6 hours after transfusion.
Rogers et al. [6] found a significant increase in infections during hospitalization in patients who received blood transfusion, and the most prevalent are the genitourinary, respiratory, digestive tract, skin and subcutaneous tissue, as well as sepsis. In this study, the risk of infections during hospitalization in transfused patients was two times higher compared to those who did not receive hemoderivatives. In this group of patients, the risk of death was five times higher in the case of elective surgery and four times higher in case of non-elective surgeries, as well as the risk of death after 30 days of hospital discharge was three times higher in patients undergoing elective surgery and four times higher in non-elective surgeries.
In Magedanz study et al. [18], in which a risk score for mediastinitis was created, an association between blood transfusion and risk of postoperative mediastinitis was found (OR: 2.5; CI95%: 1.5 - 4.1, P = 0.001), that also agrees with a study that found a strong association between transfusion and risk of infections, which reflects the immunosuppressive effect of blood transfusion [19].
The study conducted shows that transfusion of hemocomponents is directly related to increased risk of infectious processes in the postoperative period of cardiac surgery and the onset of AF during this period.
Studies have reported that blood transfusion, particularly platelets, is associated with the development of comorbidities such as AF, low cardiac output syndrome, AMI, CVA, renal failure and sepsis [14,16].
Atrial fibrillation is a common complication after cardiac surgery, ranging from 10% to 43% of the operated patients, contributing to morbidity and increased hospital stay of these patients. Koch et al. [20] in a study that evaluated the risk of developing AF in patients undergoing blood transfusion after cardiac surgery, it was concluded that transfusion is associated with the risk of AF in the postoperative period, and the risk increases for each unit transfused (OR: 1.2; 95% CI: 1.1-1.3 days; P <0.0001). Although the precise mechanism is not known, the authors speculate that the inflammatory response associated with transfusion may be exacerbated, contributing to the occurrence of AF. This may be due to leukocyte activation, leading to injury of the atrial tissue.
Some studies report that the ischemic process, blood loss and blood transfusion are known to cause severe systemic inflammatory response. Blood transfusion can also initiate a secondary inflammatory response by modifying the systemic inflammatory response of the patients and the direct introduction of bioactive substances into circulation, in addition to the primary inflammatory response initiated by the extracorporeal circulation [21-23].
In this study, patients who received hemoderivatives required longer hospital stays, however, there was no difference in mortality compared to patients who were not transfused.
In the study conducted by Hajjar et al. [7], 502 patients who underwent cardiac surgery with extracorporeal circulation (EC) were randomized to receive blood transfusion in a liberal manner (to maintain a hematocrit e" 30%) or in a more restrictive way (hematocrit e" 24%). This study demonstrates that a more conservative blood transfusion does not alter the rates of comorbidities (such as ARDS, ARF or cardiogenic shock) and mortality between the groups, demonstrating the importance of a more careful selection of patients who must undergo a blood transfusion.
In a study conducted by McGrath et al. [24], with 32,298 patients, no association between transfusion and increased morbidity and mortality after cardiac surgery was found. However, this study analyzed only the platelet transfusion, regardless of other hemoderivative components.
According to the study conducted by van Straten et al. [21], the number of units transfused may be a predictor of early mortality (up to 30 days in the postoperative period), but not of late mortality. Comparing the expected survival, the authors concluded that in patients who received three or more units of RBC, the survival rate drops significantly when compared to patients who did not receive hemoderivative products. These patients have also high incidence of postoperative complications, which could explain the high early mortality in this study.
By analyzing the relationship between blood transfusion and cardiac surgery in an older population, Veenith et al. [25] showed that blood transfusion is associated with a significant increase in mortality and length of hospital stay. The authors also report that this possible association is a result of the poor health status of patients in the preoperative period. Another factor that increases the risk of postoperative morbimortality would be that the blood transfusion may increase the risk of ischemic processes and infectious complications. This would also explain the long-term ICU and hospital stay.
Some studies also report strategies for reducing the use of hemoderivatives in postoperative cardiac surgery. Some authors report the importance of a careful preoperative evaluation, because it can reduce the risk of bleeding and the need for blood transfusion during the postoperative period. The measurement of serum iron and iron administration and preoperative erythropoietin may reduce the need for hemoderivatives. The perioperative interventions play an important role in reducing the risk of bleeding during and after surgery [4]. The use of antifibrinolytic, such as aprotinin, attenuates the systemic inflammatory response in patients undergoing EC [26]. The use of miniEC (reduction of the prime, the tubes and vacuum drainage) and the use of centrifugal pumps (Bio Pump) can reduce the excessive use of heparin [27,28]. Hypothermia (between 30º and 32º C) during the surgical procedure may also reduce bleeding during surgery and in the postoperative period. The autologous blood donation is another method used, but still requires further studies, when the patient's blood is collected prior to surgery in order to be used after the procedure. It is considered a simple, inexpensive, safe and effective method to reduce homologous blood transfusion in a wide variety of elective surgical procedures, including cardiac surgeries [4.29].
New hemoconcentration techniques during EC have also been studied. Souza & Braille [30] propose a new method of hemoconcentration, which revealed a reduction of blood and plasma used during and after EC, as well as a reduced water balance compared to the group that did not use the hemoconcentrator.
In this study, however, there were some limitations. The number of units that were transfused in each patient or the effects of other hemoderivatives in the postoperative period was not taken into consideration. Another factor that was not taken into account was the storage time of the blood transfusion bags. Thus, we conclude that the data collected revealed a tendency demonstrating that more detailed studies are needed to show the effects of each hemocomponent transfused in patients undergoing cardiac surgery.
CONCLUSION
The analysis of this study results shows that blood transfusion is associated with increased risk of infectious events (such as mediastinitis, respiratory infection, sepsis), risk of developing AF, ARF, CVA and ARDS. The blood transfusion increased the length of hospital stay, but not mortality in these patients.
REFERENCES
1. Ministério da Saúde (Brasil). Secretaria de Atenção à Saúde. Departamento de Atenção Especializada. Guia para o uso de hemocomponentes. Série A. Normas e Manuais Técnicos. Brasília: Ministério da Saúde;2008. 140p.
2. Alghamdi AA, Davis A, Brister S, Corey P, Logan A. Development and validation of Transfusion Risk Understanding Scoring Tool (TRUST) to stratify cardiac surgery patients according to their blood transfusion needs. Transfusion. 2006;46(7):1120-9. [MedLine]
3. Ferraris VA, Ferraris SP. Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J. 1995;22(3):216-30. [MedLine]
4. Souza HJB, Moitinho RF. Estratégias para redução do uso de hemoderivados em cirurgia cardiovascular. Rev Bras Cir Cardiovasc. 2008;23(1):53-9. [MedLine] View article
5. Stover EP, Siegel LC, Parks R, Levin J, Body SC, Maddi R, et al. Variability in transfusion practice for coronary artery bypass surgery persists despite national consensus guidelines: a 24-institution study. Institutions of the Multicenter Study of Perioperative Ischemia Research Group. Anesthesiology. 1998;88(2):327-33. [MedLine]
6. Rogers MA, Blumberg N, Saint S, Langa KM, Nallamothu BK. Hospital variation in transfusion and infection after cardiac surgery: a cohort study. BMC Med. 2009;7:37. [MedLine]
7. Hajjar LA, Vincent JL, Galas FR, Nakamura RE, Silva CM, Santos MH, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304(14):1559-67. [MedLine]
8. Leal-Noval SR, Rincón-Ferrari MD, García-Curiel A, Herruzo-Avilés A, Camacho-Laraña P, Garnacho-Montero J, et al. Transfusion of blood components and postoperative infection in patients undergoing cardiac surgery. Chest. 2001;119(5):1461-8. [MedLine]
9. Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ. Effect of blood transfusion on long-term survival after cardiac operation. Ann Thorac Surg. 2002;74(4):1180-6. [MedLine]
10. Whitlock R, Crowther MA, Ng HJ. Bleeding in cardiac surgery: its prevention and treatment: an evidence-based review. Crit Care Clin. 2005;21(3):589-610. [MedLine]
11. Karkouti K, Cohen MM, McCluskey SA, Sher GD. A multivariable model for predicting the need for blood transfusion in patients undergoing first-time elective coronary bypass graft surgery. Transfusion. 2001;41(10):1193-203. [MedLine]
12. Johnson RG, Thurer RL, Kruskall MS, Sirois C, Gervino EV, Critchlow J, et all. Comparison of two transfusion strategies after elective operations for myocardial revascularization. J Thorac Surg. 1992;104(2):307-14.
13. Magovern JA, Sakert T, Benckart DH, Burkholder JA, Liebler GA, Magovern GJ Sr, et al. A model for predicting transfusion after coronary artery bypass grafting. Ann Thorac Surg. 1996;61(1):27-32. [MedLine]
14. Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34(6):1608-16. [MedLine]
15. Möhnle P, Snyder-Ramos SA, Miao Y, Kulier A, Böttiger BW, Levin J, et al; Multicenter Study of Perioperative Ischemia (McSPI) Research Group. Postoperative red blood cell transfusion and morbid outcome in uncomplicated cardiac surgery patients. Intensive Care Med. 2011;37(1):97-109. [MedLine]
16. Karkouti K, O'Farrell R, Yau TM, Beattie WS; Reducing Bleeding in Cardiac Surgery Research Group. Prediction of massive blood transfusion in cardiac surgery. Can J Anaesth. 2006;53(8):781-94. [MedLine]
17. Koch C, Li L, Figueroa P, Mihaljevic T, Svensson L, Blackstone EH. Transfusion and pulmonary morbidity after cardiac surgery. Ann Thorac Surg. 2009;88(5):1410-8. [MedLine]
18. Magedanz EH, Bodanese LC, Guaragna JC, Albuquerque LC, Martins V, Minossi SD, et al. Risk score elaboration for mediastinitis after coronary artery bypass grafting. Rev Bras Cir Cardiovasc. 2010;25(2):154-9. [MedLine] View article
19. Friedman ND, Bull AL, Russo PL, Leder K, Reid C, Billah B, et al. An alternative scoring system to predict risk for surgical site infection complicating coronary artery bypass graft surgery. Infect Control Hosp Epidemiol. 2007;28(10):1162-8. [MedLine]
20. Koch CG, Li L, Van Wagoner DR, Duncan AI, Gillinov AM, Blackstone EH. Red cell transfusion is associated with an increased risk for postoperative atrial fibrillation. Ann Thorac Surg. 2006;82(5):1747-56. [MedLine]
21. van Straten AH, Bekker MW, Soliman Hamad MA, van Zundert AA, Martens EJ, Schönberger JP, et al. Transfusion of red blood cells: the impact on short-term and long-term survival after coronary artery bypass grafting, a ten-year follow-up. Interact Cardiovasc Thorac Surg. 2010;10(1):37-42. [MedLine]
22. Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD. Increased mortality, postoperative morbidity, and costs after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544-52. [MedLine]
23. Ranucci M. Allogeneic blood transfusions and infections after cardiac surgery. Am Heart J. 2007;153(5):e21. [MedLine]
24. McGrath T, Koch CG, Xu M, Li L, Mihaljevic T, Figueroa P, et al. Platelet transfusion in cardiac surgery does not confer increased risk for adverse morbid outcomes. Ann Thorac Surg. 2008;86(2):543-53. [MedLine]
25. Veenith T, Sharples L, Gerrard C, Valchanov K, Vuylsteke A. Survival and length of stay following blood transfusion in octogenarians following cardiac surgery. Anaesthesia. 2010;65(4):331-6. [MedLine]
26. Greilich PE, Brouse CF, Whitten CW, Chi L, Dimaio JM, Jessen ME. Antifibrinolytic therapy during cardiopulmonary bypass reduces proinflammatory cytokine levels: a randomized, double-blind, placebo-controlled study of epsilon-aminocaproic acid and aprotinin. J Thorac Cardiovasc Surg. 2003;126(5):1498-503. [MedLine]
27. Perthel M, El-Ayoubi L, Bendisch A, Laas J, Gerigk M. Clinical advantages of using mini-bypass system in terms of blood product use, postoperative bleeding and air entrainment: an in vivo clinical perspective. Eur J Cardiothorac Surg. 2007;31(6):1070-5.
28. Sellevold OF, Berg TM, Rein KA, Levang OW, Iversen OJ, Bergh K. Heparin-coated circuit during cardiopulmonary bypass. A clinical study using closed circuit, centrifugal pump and reduced heparinization. Acta Anaesthesiol Scand. 1994;38(4):372-9. [MedLine]
29. Yoda M, Nonoyama M, Shimakura T. Autologous blood donation before elective off-pump coronary artery bypass grafting. Surg Today. 2004;34(1):21-3. [MedLine]
30. Souza DD, Braile DM. Avaliação de nova técnica de hemoconcentração e da necessidade de transfusão de hemoderivados em pacientes submetidos à cirurgia cardíaca com circulação extracorpórea. Rev Bras Cir Cardiovasc. 2004;19(3):287-94. View article
Article receive on Monday, November 15, 2010
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license