Alexandre Noboru MurakamiI; Gabriela Guimarães BastonII; Mariana Ribeiro Rodero CardosoII; Carlos Henrique De MarchiII; Ulisses Alexandre CrotiII
DOI: 10.21470/1678-9741-2019-0203
ABSTRACT
Clinical data: Infant, 7 months, female, referred to our department at one month of age, suspecting of congenital heart disease for further investigation.AV = Atrioventricular
AVSD = Atrioventricular septal defect
PAPVC = Partial anomalous pulmonary venous connection
TAPVC = Total anomalous pulmonary venous connection
Clinical Data
Infant, 7 months, female, referred to our department at one month of age, suspecting of congenital heart disease due to heart murmur upon physical examination. No other signs or symptoms and no genetic syndrome were observed.
Physical examination revealed good general condition. Presence of systolic murmur 2+/6+ at upper left sternal border. Eupneic and clear lung sounds. No abdominal findings. Symmetrical peripheral pulses.
During outpatient follow-up, presented with dyspnea on exertion, therefore, diuretics were initiated. At 7 months of age, surgical repair was indicated.
Chest Radiography
Posterior-anterior chest radiography shows increased pulmonary vascular markings, more prominent in the upper lungs. Enlarged cardiac area with a cardiothoracic ratio of 0.63 (Figure 1).
Electrocardiography
Sinus rhythm, heart rate of 164 beats/min, SAQRS -60º, left anterior fascicular block and right ventricular hypertrophy (Figure 2).
Echocardiography
Situs solitus in levocardia. Abnormal venoatrial and atrioventricular connection and normal ventriculo arterial connection.
Doppler examination demonstrated presence of atrial septal defect (5 mm) with left-to-right shunt and ventricular septal defect (2 mm).
Common atrioventricular valve with two orifices, characterizing a transitional atrioventricular septal defect.
Left superior pulmonary vein draining on the brachiocephalic vein, typical of partial anomalous pulmonary venous connection (PAPVC).
To confirm the diagnosis, the patient underwent a complementary imaging examination.
Computed tomography angiography
Atrioventricular septal defect (AVSD) showing signs of right chamber, pulmonary trunk and left pulmonary artery dilatation. Partial anomalous pulmonary venous return from the upper left lobe in the brachiocephalic vein, as shown in Figure 3.
BV=brachiocephalic vein; ISV=intercostal systemic vein; LSPV=left
superior pulmonary vein

BV=brachiocephalic vein; ISV=intercostal systemic vein; LSPV=left
superior pulmonary vein
Diagnosis
AVSD represents approximately 4% of all cardiac malformations and total anomalous pulmonary venous connection (TAPVC) corresponds to 0.8% of all congenital heart diseases[1]. PAPVC was observed in 0.6% to 0.7% of autopsies[2]. Presence of left-sided PAPVC is described only in 7% of cases in a series of 236 patients[2]. Of the 132 patients who underwent repair of partial AVSD, 62 were associated with other heart defects and the association with PAPVC was not found[3]. Another study described an association between anomalous pulmonary venous return and AVSD in 7% of patients[4].
Clinical presentation depends on the type of AVSD. Due to left-to-right shunt at both atrial and ventricular level in complete AVSD and atrioventricular (AV) valve regurgitation, children will develop congestive heart failure[5]. Patients with partial AVSD can remain asymptomatic for years.
In this case, the clinical picture of heart failure was preponderant, characterized by need for diuretics and findings of complementary exams.
The echocardiogram performed by an experienced professional was fundamental to identify one of the pulmonary veins connecting anomalously to the brachiocephalic vein and not to the left atrium, which was confirmed by angiography (Figure 3). Computed tomography angiography is the gold standard for the diagnosis of PAPVC and can also evaluate postoperative complications, as demonstrated by Croti et al[6].
The patient presented with a small ventricular septal defect and should have little hemodynamic repercussion, but due to the presence of the anomalous left superior pulmonary vein connection, a greater right-side overload and increased pulmonary flow were observed, and early surgical treatment was indicated.
Operation
The operation was performed through a median sternotomy with partial thymus resection (left). Heparinization with 4 mg/kg and careful cannulation of the aorta and bicaval were performed as routine. Hypothermia at 28º Celsius with 123 minutes of cardiopulmonary bypass and 89 minutes of cross-clamping time.
Dissection of left superior pulmonary vein with drainage in the brachiocephalic vein. During dissection, a small intercostal systemic vein was found draining into the pulmonary vein, as shown in angiography (Figure 3B). Ligature and excision of the intercostal vein was performed. Opening on the anterior wall of the pulmonary vein and left atrial appendage and continuous suture with polydioxanone 7-0 between structures (Figure 4).
LAA and LSPV with 7-0 polydioxanone suture. LAA=left atrial appendage;
LSPV=left superior pulmonary vein; PT=pulmonary trunk
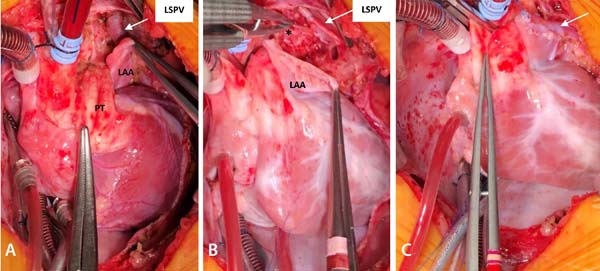
LAA and LSPV with 7-0 polydioxanone suture. LAA=left atrial appendage;
LSPV=left superior pulmonary vein; PT=pulmonary trunk
A common atrioventricular valve with two orifices and a cleft in left AV valve were found. Ventricular septal defect was single-sutured with pledgets, and the cleft in the left AV valve was closed using 6-0 polypropylene sutures. For the atrial septal defect correction, a bovine pericardium patch was used as usual. The patient had no postoperative complications, remaining 10 days hospitalized, including 6 days in a pediatric cardiac care unit and 4 days in the pediatric ward.
REFERENCES
1. Samánek M, Vorísková M. Congenital heart disease among 815,569children born between 1980 and 1990 and their 15-year survival: a prospectiveBohemia survival study. Pediatr Cardiol. 1999;20(6):411-7.doi:10.1007/s002469900502.
2. Alsoufi B, Cai S, Van Arsdell GS, Williams WG, Caldarone CA, ColesJG. Outcomes after surgical treatment of children with partial anomalouspulmonary venous connection. Ann Thorac Surg. 2007;84(6):2020-6; discussion2020-6. doi:10.1016/j.athoracsur.2007.05.046.
3. Chowdhury UK, Airan B, Malhotra A, Bisoi AK, Kalaivani M, GovindappaRM, et al. Specific issues after surgical repair of partial atrioventricularseptal defect: actuarial survival, freedom from reoperation, fate of the leftatrioventricular valve, prevalence of left ventricular outflow tractobstruction, and other events. J Thorac Cardiovasc Surg. 2009:137(3): 548-55.doi:10.1016/j.jtcvs.2008.04.035.
4. Calkoen EE, Hazekamp MG, Blom NA, Elders BB, Gittenberger-de GrootAC, Haak MC, et al. Atrioventricular septal defect.: from embryonic developmentto long-term follow-up. Int J Cardiol. 2016;202:784-95.doi:10.1016/j.ijcard.2015.09.081.
5. Christensen N, Andersen H, Garne E, Wellesley D, Addor MC, HaeuslerM, et al. Atrioventricular septal defects among infants in Europe: apopulation-based study of prevalence, associated anomalies, and survival.Cardiol Young. 2013;23(4):560-7. doi:10.1017/S1047951112001400.
6. Croti UA, Beani L, Moscardini AC, Souza Jr AS, Souza AS, SobrinhoSH, et al. Computed tomography in late evaluation of surgical treatment ofpulmonary veins total anomalous connection. Rev Bras Cir Cardiovasc.2011;26(4):532-43. doi:10.5935/1678-9741.20110042.
No financial support.
No conflict of interest.
Authors’ roles & responsibilities
ANM Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published
GGB Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; final approval of the version to be published
MRRC Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; final approval of the version to be published
CHM Final approval of the version to be published
UAC Drafting the work or revising it critically for important intellectual content; final approval of the version to be published
Article receive on Monday, April 22, 2019
Article accepted on Thursday, May 23, 2019
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license