ABSTRACT
Background: Tobacco use is an important modifiable risk factor for cardiovascular disease. Few studies have investigated the frequency of smoking cessation among patients submitted to heart surgery. Objective: To determine the frequency of smoking cessation in patients submitted to coronary artery bypass graft surgery. Methods: In this cohort study, 203 consecutive patients, aged above 18, submitted to coronary artery bypass graft surgery in the period from January 2006 to March 2007, were interviewed in relation to the use of cigarettes in the pre- and postoperative period. Smokers were stratified according to the levels of nicotine dependence with the use of Fagerström Nicotine Dependence Test. They were followed as outpatients during 60 and 90 days for the occurrence of smoking. Results: The mean age of the group was 62 ± 10 years, and 134 (66%) were male. Before surgery, 146 (71.9%) patients were smokers. A significant number of patients stopped smoking in the postoperative period: 136 (93.15%) and 137 (93.84%) on days 60 and 90, respectively, remained not smoking after surgery. Conclusion: Coronary artery bypass graft surgery is an important determinant of smoking cessation.
RESUMO
FUNDAMENTO: Tabagismo é um importante fator de risco modificável para doença cardiovascular. Poucos estudos têm investigado a frequência da cessação de fumar entre pacientes submetidos à doença cardíaca. OBJETIVOS: Determinar a frequência da cessação de fumar em pacientes submetidos à cirurgia de revascularização do miocárdio. MÉTODOS: Estudo de coorte, de 203 pacientes consecutivos, maiores de 18 anos, submetidos à cirurgia de revascularização do miocárdio no período de janeiro 2006 a março de 2007, quando foram entrevistados em relação ao uso de cigarros no período pré e pós-operatório. Fumantes foram estratificados de acordo com o grau de dependência com o uso do Teste de Dependência de Fagerström. Os pacientes foram seguidos durante 60 e 90 dias para avaliar uso de cigarros. RESULTADOS: A média de idade do grupo foi de 62 ± 10 anos, e 134 (66%) eram homens. Antes da cirurgia, 146 (71,9%) pacientes eram fumantes. Um número significativo de pacientes parou de fumar no período pós-operatório: 136 (93,15%) e 137 (93,84%), aos 60 e 90 dias, respectivamente, pararam de fumar depois da cirurgia. CONCLUSÃO: Cirurgia de revascularização do miocárdio é um importante determinador para cessação de fumar.
INTRODUCTION
Despite the anti-tobacco use campaigns, more than 1 in 10 cardiac patients died in the world in 2000 due to causes related to tobacco use, showing that it is an important cause of cardiovascular mortality [1]. Patients that kept on smoking after the coronary artery bypass graft surgery (CABGS) present higher risk of death than those patients ceased smoking. They are also submitted to procedures of revascularization more frequently [2]. In spite of these perspectives, quitting smoking is a challenge for many people. Although it is estimated that 70% of smokers worldwide would like to get rid of their addiction, only one third has success each year [3,4]. Several psychotherapy approaches, associated or not to pharmacologic treatments such as reposition of nicotine or bupropion, have been used, showing evidences of 10%-25% of efficiency in different clinical experiments [5]. It becomes a must to identify situations and strategies that can improve the efficiency of treatments for tobacco use. In all therapy approaches, cease smoking is one of the most crucial factors [6]. Crisis situations and events involving serious health risks, such as acute infarction of the myocardium, hospitalization, surgery and loss of relatives due to tobacco use related diseases, may represent an important motivation in order to cease smoking [7-14].
A limited number of studies have shown that CABGS in patients with ischemic disease represent a strong influence in order to cease smoking [15-18]. The factors involving these situations and the degree of nicotine addiction in this group of patients are not well understood. This study aimed to investigate the frequency of smoking cessation between patients submitted to CABGS.
METHODS
This prospective cohort analyzed 203 consecutive patients submitted to CABGS, between January, 2006 and March, 2007 (in the preoperative and postoperative periods), in three University Hospitals: Instituto de Cardiologia do Rio Grande do Sul (ICRS), Hospital de Clínicas de Porto Alegre (HCPA) and Irmandade Santa Casa de Misericórdia de Porto Alegre (ISCM). All adult patients, of both genders, and receiving medical care in each hospital. The professionals involved in the therapy procedures were not aware of the research project. There was no systematic approach for smoking cessation with these patients.
The study was approved by the Ethics Committee of the three hospitals involved. The patients that agreed to take part in this study signed up an agreement term. Patients were interviewed 60 and 90 days after CABGS regarding smoking cessation incidence. Further information was acquired through medical leaflets.
Patients operated in emergency or holding acute coronary syndrome or concomitant congenital heart disease and valve surgery were excluded from this study.
Research tools
Patients answered a questionnaire structured on demographic, anthropometric and clinical data. The Fagerström Nicotine Dependence Test (FNDT) [19,20] was created in 1978 and validated in Brazil by Carmo & Pueyo, being used to determine the degree of nicotine addiction [18]. The patients were rated according to the FNDT [19]. By using the FNDT, patients were stratified in three groups, according to the degree of nicotine dependence: a. very low and low; b. moderate; c. very high and high.
For analysis purposes, the patients stratified according to the degree of nicotine dependence by the Fagerström Test were allocated in three groups: a. very low and low degree; b. moderate degree; c. high and very high degree. The tobacco users were classified by the following criteria: a. present smoker (smoking from the date of surgery to one year earlier); b. in abstinence (smoking cessation from 1 to 20 years); c. ex-smokers (smoking cessation over 20 years); d. passive smokers (cohabiting with a smoker)[14,21]. The surgical risk was determined by a clinical risk score of the Cleveland Clinic [22].
Statistical analysis
The data collected were analyzed by the SPSS (I) Program version 15.0. The categorical variables are presented by absolute frequencies and percentages and the continuous variables with normal distribution, by mean or standard deviation, whereas those without normal distribution, by mean and interquartilic amplitude (IQ).
In order to evaluate the demographic, anthropometric and clinical characteristics of the patients regarding smoking and complications, it was applied a Student's t test, for the continuous variables with symmetrical distribution, or the Mann-Whitney's test, for the variables with asymmetrical distribution, and the chi-square test or Fisher's exact test, for the categorical variables.
The logistic regression was used in order to control confusing factors and evaluate postoperative complication predictors.
The variables with
P ≤ 0.20 were used in the logistic regression model for the analysis of smoking associated with postoperative complicacies in 60 days.
In all analyses a value
P ≤ 0.05 was considered statistically significant.
RESULTS
Sample characteristics
There were selected 211 consecutive patients in the preoperative of CABGS. Eight patients were excluded for not having undergone surgery for different reasons. The sample of the study, thus, consisted of 203 patients, being 134(66%) male, with mean age 62±10 years. Average income was US$ 340.00 (US$ 198.00 - US$ 592.00) and 146(71.9%) patients were smokers.
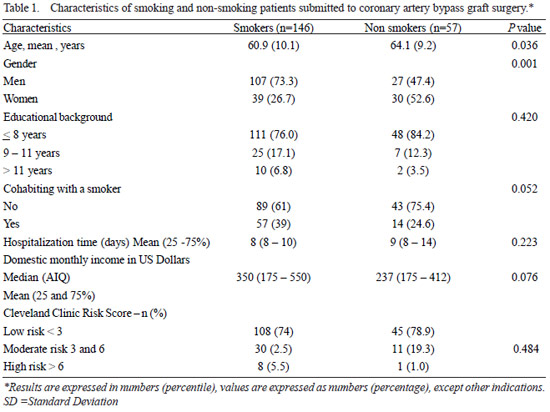
General characteristics of the sample are presented on Table 1. The groups were different, for the smoking group presented lower age patients, higher number of male patients, tendency of higher income, cohabiting with tobacco users and educational background.
There was a significant cessation of smoking in the postoperative. Out of 146 smoking patients prior to surgery, only 10(6.85%) and nine (6.16%) continued smoking after CABGS.
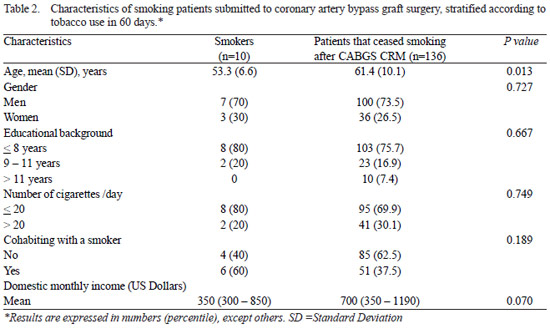
The general characteristics of these patients are presented in Table 2. Patients that continued smoking presented lower age and income.
Figure 1 shows the Fagerström classification, in which patients were rated prior to CABGS, in 60 and 90 days after CABGS. The percentage of smoking cessation was also analyzed in 60 and 90 days in the stratified group according to the degree of tobacco use addiction. An expressive cessation was observed in all groups. Considering the small number of patients that kept on smoking, it cannot be observed a correlation between the degree of addiction and cessation in the postoperative (Figure 1).
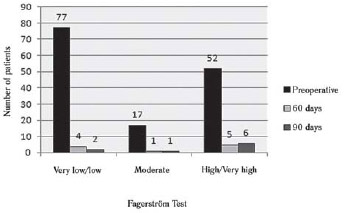
Fig. 1 - Distribution of smoking patients, stratified according the degree of tobacco addiction, during the preoperative period and 60 and 90 days after coronary artery bypass graft surgery
This study showed that a large number of patients quit smoking within 60 or 90 days after CABGS. This percentage of smoking cessation, (93.15%) was higher than initially expected. It was the highest result ever observed so far with efficient behavioral and pharmacologic approaches observed in different studies, in which the rates ranged from 10%-25% [15-18]. Our results compared to those of other studies showed high percentile of smoking cessation in patients hospitalized for CABGS. Hilleman et al. [23] studied a sample of patients submitted to CABGS and observed that 85% quit smoking. Rigotti et al. [16] performed a random controlled clinical study following patients submitted to CABGS for a year and 94% of the patients were followed up for a period of 5.5 years, in order to check the efficiency of a smoking cessation program in patients submitted to CABGS. The results showed that, even without a specific intervention, almost half of the smoking patients cease smoking, for five years, after heart surgery.
In this study there were not observed significant differences between the different degrees of nicotine dependence, in the behavior of ceasing tobacco use in the postoperative. The number of patients that kept their smoking habit was very low and, thus, that could not be inferred as the degree of addiction shows correlation or not with smoking cessation in the postoperative. Cavender et al. [24] performed a random controlled clinical study, in which the magnitude and the profile of nicotine dependence among patients submitted to CABGS were determined by the FNDT. According to the test and the patient's preferences, it was set up a customized nicotine reposition treatment, with planned duration. The percentage of smoking cessation was not correlated with the degree of nicotine dependence.
The results observed in the present study could have different causes. Crisis situations, such as hospitalization, may motivate patients to quit smoking. CABGS is associated to a very high percentile of smoking cessation in a short period of follow-up. The hospitalization period and the follow-up of these patients can be used by a multidisciplinary crew in order to motivate them and their relatives to quit smoking.
The multidisciplinary crew could look after these patients during the hospitalization period, which could contribute during the postoperative period. The total results were positive for a large percentile of patients that quit smoking. This study suggests that smoking cessation programs may stimulate the cessation of tobacco use in the postoperative and its benefits in a long period of follow-up [15,18].
CONCLUSION
The coronary artery bypass graft surgery is an important determining factor for smoking cessation.
REFERENCES
1. Ezzati M, Henley SJ, Thun MJ, Lopez AD. Role of smoking in global and regional cardiovascular mortality. Circulation. 2005;112(4):489-97. [MedLine]
2. Van Domburg RT, Meeter K, van Berkel DF, Veldkamp RF, van Herwerden LA, Bogers AJ. Smoking cessation reduces mortality after coronary artery bypass surgery: a 20-year follow-up study. J Am Coll Cardiol. 2000;36(3):878-83. [MedLine]
3. Rigotti NA. Clinical practice. Treatment of tobacco use and dependence. N Engl J Med. 2002;346(7):506-12. [MedLine]
4. Myles PS, Iacono GA, Hunt JO, Fletcher H, Morris J, McIlroy D, et al. Risk of respiratory complications and wound infection in patients undergoing ambulatory surgery: smokers versus nonsmokers. Anesthesiology. 2002;97(4):842-7. [MedLine]
5. Barth J, Critchley J, Bengel J. Efficacy of psychosocial interventions for smoking cessation in patients with coronary heart disease: a systematic review and meta-analysis. Ann Behav Med. 2006;32(1):10-20. [MedLine]
6. NIH State-of-the-Science Panel. National Institutes of Health State-of-the-Science conference statement: tobacco use: prevention, cessation, and control. Ann Intern Med. 2006;145(11):839-44. [MedLine]
7. Warner DO. Helping surgical patients quit smoking: why, when, and how. Anesth Analg. 2005;101(2):481-7.
8. Marques ACPR, Campana A, Gigliotti AP, Lourenço MTC, Ferreira MP, Laranjeira R. Consenso sobre o tratamento da dependência de nicotina. Rev Bras Psiquiatr. 2001;23(4):200-14.
9. Costa AA, Elabras JF,Araújo ML, Ferreira JES, Meirelles LR, Magalhães CK. Programa multiprofissional de controle do tabagismo: aspectos relacionados à abstinência de longo prazo. Rev SOCERJ. 2006;19(5):397-403.
10. Tonstad S, Andrew Johnston J. Cardiovascular risks associated with smoking: a review for clinicians. Eur J Cardiovasc Prev Rehabil. 2006;13(4):507-14. [MedLine]
11. Rigotti NA, Arnsten JH, McKool KM, Wood-Reid KM, Pasternak RC, Singer DE. Efficacy of a smoking cessation program for hospital patients. Arch Intern Med. 1997;157(22):2653-60. [MedLine]
12. Sciamanna CN, Hoch JS, Duke GC, Fogle MN, Ford DE. Comparison of five measures of motivation to quit smoking among a sample of hospitalized smokers. J Gen Intern Med. 2000;15(1):16-23. [MedLine]
13. Munafò M, Rigotti N, Lancaster T, Stead L, Murphy M. Interventions for smoking cessation in hospitalised patients: a systematic review. Thorax. 2001;56(8):656-63. [MedLine]
14. Trigo M, Rocha E. Cessação de hábitos tabágicos em doentes coronários. Acta Med Port. 2002;15:337-44. [MedLine]
15. Hajek P, Taylor TZ, Mills P. Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: randomised controlled trial. BMJ. 2002;324(7329):87-9. [MedLine]
16. Rigotti NA, McKool KM, Shiffman S. Predictors of smoking cessation after coronary artery bypass graft surgery. Results of a randomized trial with 5-year follow-up. Ann Intern Med. 1994;120(4):287-93. [MedLine]
17. Simon JA, Solkowitz SN, Carmody TP, Browner WS. Smoking cessation after surgery: a randomized trial. Arch Intern Med. 1997;157(12):1371-6. [MedLine]
18. Quist-Paulsen P, Bakke PS, Gallefoss F. Predictors of smoking cessation in patients admitted for acute coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005;12(5):472-7. [MedLine]
19. Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav. 1978;3(3-4):235-41. [MedLine]
20. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119-27. [MedLine]
21. Strecher VJ, Shiffman S, West R. Moderators and mediators of a web-based computer-tailored smoking cessation program among nicotine patch users. Nicotine Tob Res. 2006;8(Suppl 1):S95-101. [MedLine]
22. Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992;267(17):2344-8. [MedLine]
23. Hilleman DE, Mohiuddin SM, Packard KA. Comparison of conservative and aggressive smoking cessation treatment strategies following coronary artery bypass graft surgery. Chest. 2004;125(2):435-8. [MedLine]
24. Cavender JB, Rogers WJ, Fisher LD, Gersh BJ, Coggin CJ, Myers WO. Effects of smoking on survival and morbidity in pacients randomized to medical or surgical therapy in the Coronary Artery Surgery Study (CASS): 10-year follow-up. CASS Investigators. J Am Coll Cardiol. 1992;20(2):287-94. [MedLine]
Article receive on Monday, September 21, 2009
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license