The case of an eleven-month-old female child is presented diagnosed as having congenital heart disease with pulmonary hyperflow, who was submitted to a surgery to close an interventricular communication, interatrial communication and arterial canal ligature. The infant evolved with persistent atelectasis at the right lung base in the postoperative period which did not respond to conventional physiotherapeutic measures. Inhalation of hypertonic saline solution with 6% NaCl was associated as a coadjuvant therapy, giving a total cure of the atelectasis after three days of treatment.
Criança de 11 meses, sexo feminino, submetida à operação de fechamento de comunicação interventricular, comunicação interatrial e ligadura de canal arterial. Evoluiu no pós-operatório com atelectasia persistente em base pulmonar à direita, não respondendo às manobras fisioterapêuticas convencionais, efetuadas seis vezes ao dia. Após associação, como coadjuvante, da inalação de solução salina hipertônica com NaCl a 6%, imediatamente antes e após o atendimento fisioterápico, observou-se crises de tosse produtiva, com maior indução do escarro e resolução completa da atelectasia, com três dias de tratamento.
INTRODUCTION
Atelectasis is described as a state of a determined region of collapsed and non-ventilated pulmonary parenchyma associated to a loss in pulmonary volume and capacity, diagnosed by clinical and complimentary examinations [1]. This corresponds to 80% of pulmonary complications in the postoperative period of cardiovascular surgery [2].
Conventional physiotherapy frequently prevents atelectasis however, in some cases it is insufficient and there is a necessity of an association with alternative methods [3]. One coadjuvant option is the inhalation of hypertonic saline solution (HSS) with 6% sodium chloride (NaCl) as it induces productive coughing with a greater quantity of phlegm due to an increase in the mucociliary clearance [4].
Due to the positive effects of HSS, this report aims at demonstrating the effectiveness of the association of respiratory physiotherapy with the inhalation of 6% NaCl HSS in persistent atelectasis following pediatric heart surgery.
CASE REPORT
An 11-year-old girl with a history of congenital heart disease involving pulmonary hyperflow is reported. A right ventricle inflow tract perimembranous interventricular communication, an interatrial foramen ovale type communication, slight mitral valve insufficiency and pulmonary hypertension were diagnosed by echocardiogram.
The patient was accompanied in the pediatric outpatients' clinic of Hospital de Base in São José do Rio Preto from seven months old with the condition evolving to grade III congestive heart failure (NYHA) even with the use of diuretics, digitalis and an angiotensin converting enzyme inhibitor.
The child was submitted to a surgery to correct the defects with the closure of the interventricular communication using a bovine pericardium patch, closure of the interatrial communication by direct suturing and double ligature of the arterial duct. The time of cardiopulmonary bypass was 77 minutes and myocardial ischemia time was 48 minutes.
The patient was transferred to the intensive care unit (ICU) under mechanical respiration on the 2nd postoperative day presenting with pulmonary arterial hypertension which became constant implicating a necessity to remain intubated with a prolongation of the mechanical ventilation. During her stay in the ICU there was a significant increase in the amount of pulmonary secretion with extubation only being possible on the 8th postoperative day. Three days later, at chest radiograph, a hypointense region was identified at the base of the right lung with displacement of the ipsilateral mediastinum and, thus, right basal atelectasis was diagnosed (Figure 1).

Fig. 1 - Chest radiogram in the posteroanterior position on the 13th postoperative day showing right basal atelectasis
Chest radiographs were performed daily as were four 20-minute sessions of respiratory physiotherapy utilizing pulmonary re-expansion maneuvers and bronchial hygiene with selective bronchial postural drainage and tracheal suction.
After evidencing the persistence of the atelectasis, respiratory physiotherapy was intensified to six sessions daily (the maximum number of sessions that the service could offer) but without improvement in the patient's condition.
On the 13th day, therapy using inhalation of 5 mL of 6% NaCl HSS was added immediately before and after the aforementioned physiotherapeutic sessions with the belief that there would be an increase in productive coughing even though there was a possibility that the patient would present with thoracic pain in the postoperative period due to the effort, for which painkillers were prescribed. Prior to initiating the treatment, it was discussed with the child's parents.
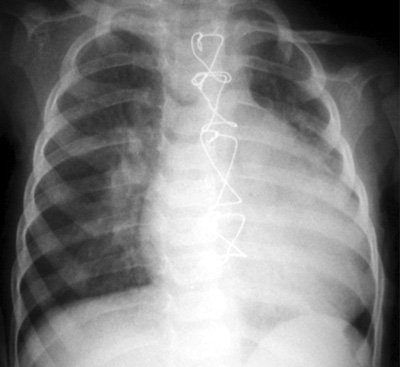
Within three days there was total resolution of the atelectasis with a significant improvement of the lung which was clearly attributed to the association of techniques (Figure 2).
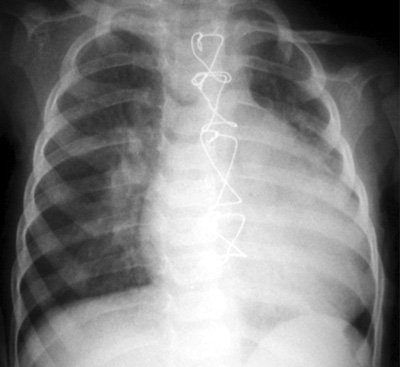
Fig. 2 - Chest radiogram in the posteroanterior position on the 16th postoperative day showing clear improvement of the right basal atelectasis
Atelectasis alters the pulmonary mechanics leading to reductions in the residual volume, vital capacity, residual function and total pulmonary capacity. Usually it is a secondary manifestation and not a primary disease. It can occur in three ways: compression of the parenchyma due to intra- or extra-thoracic processes; increase in the surface tension of the alveoli and/or bronchioles and obstruction of the airways [3]. In this infant, it is accredited that the latter associated with an accumulation of secretions was the cause of atelectasis.
Atelectasis is a common complication in the postoperative period of pediatric heart surgery and also commonly seen in the ICU. When serial chest radiographs identify atelectasis after surgery and extubation of children, efficacious methods are sometimes required as conventional physiotherapy is insufficient to reverse the state.
Hypoventilation is one of the most common causes of atelectasis in the postoperative period. With the use of anesthesia, narcotic drugs and ventilation arrest during the operative procedure and with the use of a cardiopulmonary bypass associated with pain, there is a decrease in the ciliary function, limitation of the inspiratory effort and harm to the efficiency of coughing favoring the accumulation of pulmonary secretions [5]. This patient remained under cardiopulmonary bypass for 77 minutes using anesthetics and narcotic drugs, associated with pain in the postoperative period affecting the pulmonary function which facilitated the accumulation of secretions and hypoventilation.
Bronchial hygiene and pulmonary expansion maneuvers, active or assisted respiratory kinesitherapy, selective bronchial postural drainage, incentive inspirometers, expiratory resistors with positive expiratory pressure, coughing or endotracheal suction and changes in position [3,6] were insufficient to reverse the atelectasis. Thus it was necessary to associate another method to improve the efficaciousness of the pulmonary treatment.
Since the 1980s, induction of phlegm by the inhalation of HSS has been used [4] and has proved to be safe for both children and teenagers [7]. HSS is commercially found in concentrations of 0.9%, 9% and 20%. Studies show that the most efficacious concentrations for this type of complication are concentrations of about 6% [8]. After several inhalations of 6% NaCl HSS the child presents with productive coughing crises showing its efficacy at inducing the clearance of phlegm.
Inhalation of 6% NaCl HSS is known to accelerate tracheal-bronchial clearance in many different conditions, probably by inducing osmosis to the inside of the airways, accelerating the reology of the mucous thereby favoring mucociliary clearance [8]. The best mucociliary clearance is attained with the inhalation of HSS at concentrations of between 3% and 12% with the effect dependent on the dose [9,10]. The tolerance limit is 12% as higher concentrations may cause pharyngeal irritation and at a concentration of 14.4% the ciliostatic effect is irreversible [10].
In this case, it was observed that inhalation of HSS facilitated the removal of phlegm as it was associated with physiotherapeutic maneuvers to impel the secretion to the upper airways. As the excess of secretion was probably the cause of reverse atelectasis, these data corroborate with prior publications.
A concentration of 6% was chosen as there were no publications on the postoperative period of pediatric heart surgery and we believed that this concentration would be harmless and adequate but without causing adverse effects to the patient. However, further studies with a larger number of patients are necessary to evaluate the pulmonary parameters and verify the long-term effects and its impact on morbidity and mortality rates.
CONCLUSION
The inhalation of hypertonic saline solution with 6% NaCl associated with conventional respiratory physiotherapy proved to be efficacious in this patient who had presented with difficult to treat atelectasis. Thus, this coadjuvant option can be considered in the treatment of lungs in the postoperative period of pediatric heart surgery.
REFERENCES
1. Schindler MB. Treatment of atelectasis: where is the evidence? Crit Care. 2005;9(4):341-2.
2. Andrejaitiene J, Sirvinskas E, Bolys R. The influence of cardiopulmonary bypass on respiratory dysfunction in early postoperative period. Medicina (Kaunas). 2004;40(Suppl 1):7-12.
3. Pasquina P, Merlani P, Granier JM, Ricou B. Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesth Analg. 2004;99(4):1001-8.
4. Scheicher ME, Terra Filho J, Vianna EO. Indução de escarro: revisão de literatura e proposta de protocolo. São Paulo Med J. 2003;121(5):213-9.
5. Strandberg B. The incidence of atelectasis after heart operations with and without breathing exercises. Ann Phys Med 1956;3(1):18-20.
6. Westerdahl E, Lindmark B, Eriksson T, Hedenstierna G, Tenling A. The immediate effects of deep breathing exercises on atelectasis and oxygenation after cardiac surgery. Scand Cardiovasc J. 2003;37(6):363-7.
7. Palomino AL, Bussamra MH, Saraiva-Romanholo BM, Martins MA, Nunes MP, Rodrigues JC. Escarro induzido em crianças e adolescentes com asma: segurança, aplicabilidade clínica e perfil de células inflamatórias em pacientes estáveis e durante exacerbação. J Pediatr. 2005;81(3):216-24.
8. Middleton PG, Pollard KA, Wheatley JR. Hypertonic saline alters ion transport across the human airway epithelium. Eur Respir J. 2001;17(2):195-9.
9. Daviskas E, Anderson SD, Gonda I, Eberl S, Meikle S, Seale JP, et al. Inhalation of hypertonic saline aerosol enhances mucociliary clearance in asthmatic and health subjects. Eur Respir J. 1996;9(4):725-32.
10. Boek WM, Keles N, Graamans K, Huizing EH. Physiologic and hypertonic saline solutions impair ciliary activity in vitro. Laryngoscope. 1999;109(3):396-9.

 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license