Patients undergo to cardiac surgery have more probability to develop thrombocytopenia. The heparin induced thrombocytopenia happens in 5% of the patients. The aim from this study was to evaluate the clinical importance from the severe thrombocytopenia in postoperative cardiac surgical patients.
during firsts 24 h from postoperative. All patients underwent evaluation for four Ts score (thrombocytopenia, use preview of heparin, thrombosis and platelets decreased not related to heparin). In order to a four Ts score e? 6 was considered as suggestive of heparin induced thrombocytopenia type II. The mortality rate in intensive care (ICU) and hospital, length of stay, healthy state and incidence from thrombosis were compared in patients with score
6 (group 1) and < 6 (group 2).
It was include 120 patients who met the inclusions criterions. There was no difference between the groups in related to age, gender, time of cardiopulmonary bypass and surgery. However, the incidence of thrombosis was higher in group 1 (23% vs. 0%,
<0.0001), as well as the greater score is related to higher hospital mortality rate.
6, in postoperative cardiac surgical patients, it is associated to higher incidence of thrombosis as well as the greater score is related to higher hospital mortality rate.
Pacientes submetidos à cirurgia cardíaca estão mais propensos a desenvolver plaquetopenia. A trombocitopenia induzida por heparina acomete cerca de 5% dos pacientes. O objetivo foi avaliar a importância clínica da trombocitopenia grave em pacientes no pós-operatório de cirurgia cardíaca.
Estudo prospectivo observacional que incluiu os pacientes de cirurgia cardíaca com plaquetas <150.000 cel/mm
, durante as primeiras 24 h do pós-operatório. Todos os pacientes foram submetidos a avaliação pelo escore dos quatro “Ts” (trombocitopenia, uso de heparina prévia, trombose e queda de plaquetas não relacionada à heparina) e considerado como suspeita de trombocitopenia induzida pela heparina tipo II um escore
6. A mortalidade na Unidade de Terapia Intensiva (UTI) e hospitalar, o tempo de internação, os escores de gravidade e a incidência de tromboses foram comparados em pacientes com escore e” 6 (grupo 1) e < 6 (grupo 2).
Foram incluídos 120 pacientes divididos nos dois grupos, não havendo diferença entre os mesmos com relação a idade, prevalência do sexo, tempo de circulação extracorpórea e de cirurgia. Contudo, a incidência de trombose foi mais elevada nos pacientes do grupo 1 (23% vs. 0%,
<0,001).
6, em pacientes no pós-operatório de cirurgia cardíaca, está associado a maior incidência de trombose, assim como o maior escore está relacionado à elevada mortalidade hospitalar.
INTRODUCTION
Thrombocytopenia is a common problem in severe patients, reaching 35% of high-risk surgical patients during postoperative period and 23% of clinical patients, and 8% of them need platelet transfusions [1,2]. Patients undergoing cardiac surgery has a high probability of developing thrombocytopenia, from 35% to 65% of the patients. A recognized cause of thrombocytopenia, among many, is the heparin-induced thrombocytopenia (HIT) that has two types: I - caused by direct interaction between heparin and platelets, with no immunologic etiology and appears very early; II - caused by immune reaction mediated by antibodies which react with the heparin-platelet factor 4 complex and, bind themselves to the platelets surface to induce the important thrombocytopenias [3-5].
Despite the HIT type II adversely affect the prognosis of patients [6-9], some studies show that it is a underdiagnosed disease in medical practice, and even when it is recognized, there is a delay in the suspension of heparin [10]. This scenario may demonstrate the diagnosis difficulty that combines clinical and laboratory criteria, even greater difficulty in patients undergoing cardiac surgery with other reasons to justify thrombocytopenia [60-10].
Considering the impact of this disease on patients evolution and the cost it has for the health system [11,12], it is pertinent to investigate whether the commonly used score (4Ts [13.14] - Table 1) for the diagnosis would be sufficient as initial prognostic assessment of patients undergoing cardiac surgery who develop HIT, as well as the clinical importance of thrombocytopenia in postoperative period of cardiac surgery. Assim como, a importância clínica da trombocitopenia em pós-operatório de cirurgia cardíaca.
Therefore, this study aims to evaluate the clinical importance of thrombocytopenia in patients during the postoperative period after cardiac surgery.
METHODS
This was a prospective observational cohort study in adult patients in the postoperative period of cardiac surgery, from December 2006 to December 2007, in the general ICU at a tertiary hospital.
This is a specialized unit that monitors the critically ill, clinical and surgical patients, consisting of 20 beds, with residents providing care to hospitalized patients under the supervision of physician assistants.
Once approved by the Research Ethics Committee of this institution and with a signed informed consent, all patients consecutively admitted to ICU for postoperative care of cardiac surgery with extracorporeal circulation (EC) and with value of platelets <150,000 cells/mm3, were included in the study, dur ing the immediate postoperative period (from admission until 6 am the day after surgery).
During the intraoperative period, all patients underwent heparinization with bovine heparin at a dose of 4 mg / kg of body weight, as well as the oxygenators were all the same brand and all of them operated with roller pumps.
All patients were evaluated with 4ts score [13] to detect suspected HIT II. score
> 6 was considered as suspected HIT II [13].
The 4Ts score is defined as score 0-2 for each of the following criteria: thrombocytopenia with falling platelet counts more than 30% from baseline, onset time of falling platelets after the use of heparin, the occurrence of thrombosis and other causes of falling platelet counts unrelated to heparin (Table 1) [13,14].
Patients younger than 18 years of age were excluded from the study and all were followed-up until hospital discharge or death.
The active searches for patients and data collection were performed by physicians specially trained to control possible errors. In order to standardize data collection, the worst values + of physiological and laboratory variables were used for calculation of APACHE II (Acute Physiology And Chronic Health Evaluation) [15], SOFA (Sequential Organ Failure Assessment) [16] and MODS (multiple-organ dysfunction Syndrome) [17]. Researchers did not have any influence on patient treatment.
Data were entered into an electronic database (Microsoft Excel) and subsequently analyzed through a statistical program (SPSS).
Demographic data were expressed as mean ± standard deviation, median and interquartile range or as percentage. All statistical tests were two-tailed and significance level of 0.05 was used. Quantitative variables with normal distribution were analyzed through parametric methods (Student T), and qualitative variables with irregular distribution via non-parametric tests (Chi-square, Fisher's exact and Mann Whitney tests).
This study had no external funding sources.
RESULTS
There were 120 patients who studied with platelet count in the immediate postoperative period <150,000 cells/mm3, and 59.2% of them were male, aged 63 ± 10 years.
The mean APACHE II, SOFA and MODS were respectively 16.4 ± 4.8, 6.1 ± 2.4 and 6.7 ± 2.0. hospital mortality was 20.8%. (table 2)
Coronary artery bypass graft was the most frequent surgery with prevalence of 60.0% (Table 2). The 4Ts median was 5 (4-6), 47.6% had scores greater than or equal to 6 (Figure 1).

Fig. 1 - Frequency of 4TS score among patients
2
Demographics data, mortality rates, thrombosis and ICU stay were evaluated among patients with scores
> 6 and <6 in the univariate analysis. (table 3). there was significant difference among the scores, sofa and mods variables, platelet and thrombosis. enquanto o tipo e tempo de cirurgia, tempo de cec não apresentaram diferença estatisticamente significante entre os grupos.
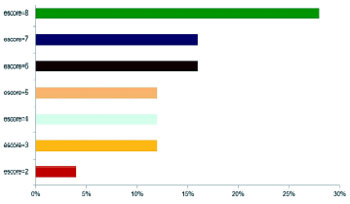
Patients with higher 4Ts scores had greater hospital mortality rates with significant difference (
P <0.001). (figure 2).
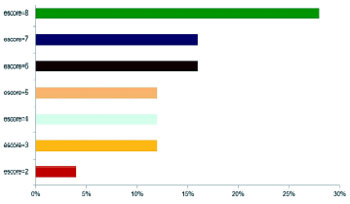
Fig. 2 - Percentage of hospital mortality compared with 4TS score. X
2 Linear tendency
Heparin has been used for over 50 years for prevention and treatment of venous thrombosis. The main adverse effect of this medication is the bleeding that occurs in 1% to 33% of patients [18]. In addition to this, there are other important adverse effects, such as: heparin-induced thrombocytopenia (HIT), osteoporosis, eosinophilia, hypercalcemia, cutaneous reaction and other allergic reactions other than HIT [18].
Weismann & Tobin, in 1958 [19] and Roberts et al., in 1964 [20] were the first ones to describe the thrombotic effects in some patients receiving heparin for 7-14 days. Two distinct types of HIT are described: the first is reversible and does not involve the immune process (type I), while the second is mediated by reaction with immunoglobulin G antibody (type II) and evolves with a worse prognosis [6].
The literature shows how the expected death rate for patients undergoing CABG from 3% to 5% [21], while in this study hospital mortality was 20.8%, however, we must consider that this sample is from patients with thrombocytopenia lower than 150,000 cells/mm3. In this sample, 47.6% of patients achieved 4Ts score
> 6, thus more likely to present with HIT type II [13], explaining the poorest performance, since those patients who are undergoing cardiac surgery and have HIT type II, 44% of them evolve with thromboembolic complications and 33% die [22,23]. Moreover, the mortality rate predicted by the mean APACHE II (16.4) of the study population is 23.5%.
The type of heparin used did not reduce the incidence of thrombosis or the highest score obtained by patients and, the opposite was observed in the literature, where the risk of HIT II decreases from 80 to 10 times in patients receiving low molecular weight heparin [10, 11.24]. However, all patients received unfractionated heparin during surgery that may have influenced the results in this sample.
In patients with 4Ts score
> 6, there were more mortalities in hospital and ICU, with a strong tendency statistically significant. There were no differences in severity when groups with scores
> 6 and <6 compared to APACHE II, therefore it is impossible to justify the increased mortality in the group score
> 6 for the patient's condition. As the surgical time, extracorporeal circulation, type of surgery, prior use of acetylsalicylic acid, reoperation, transfusion, metabolic variables or stays in the ICU and hospital, since these variables were also not different among the groups.
The incidence of thrombosis in the group with a score
> 6 was much higher, even with lower platelets serum levels. The thrombotic events observed were as severe as cerebrovascular accident, acute myocardial infarction, pulmonary thromboembolism, deep venous, mesenteric, venous sinus and microvascular thromboses.
In addition, it was observed that the higher 4Ts score were, worse the patients' prognosis are, the mortality in patients with a score of 8 was 30%, ten times higher than in patients with scores from 2 to 3% of death, a difference that was significant (P <0.001). it is also important to emphasize the importance of clinical diagnosis of HIT II, as well as prognostic evaluation.
The available data are enough for consensus of the issue relevance in the evolution of these patients, however, despite the extensive descriptions in the literature, consensus and guidelines attempting to regulate the conduct [6-9,25,26], a registration study [10] shows alarming data: HIT was suspected in only 20% of patients with thrombocytopenia; heparin was discontinued in only 30% of patients with suspected HIT, death and thrombotic complications occurred in 30% of patients who were using heparin, less than 10% of patients with thrombocytopenia had a diagnostic evaluation for HIT.
Facing this scenario, the current study becomes more relevant as there is an objective to evaluate the clinical importance of HIT in a high-risk group, by using a simple tool for diagnosis and also considering this tool a perspective of prognostic assessment.
Some study limitations should be considered, the observational design with the inherent restrictions to this type of study and, due to this reason, further studies are needed. it is too precocious for the thrombocytopenia to be considered as HIT [27], however we cannot ignore that the patients were exposed to heparin for a longer period, because the median hospital stay before surgery was 8 days. HIT occurs after the fifth day of the heparin start, however, in patients with previous use it may occur on the first day [28], furthermore, a small dose of heparin can cause immune sensitization to subsequent exposure to heparin. [29]
The type of unfractionated heparin (bovine) used in this study is a limitation [30], since it has been associated with higher incidence of antibodies against the heparinplatelet factor 4 complex [31].
Another issue is the absence of a laboratory evaluation with doses of anti-platelet factor 4 / heparin, once the gold standard for diagnosis is clinical criterion associated with a laboratory confirmation [5.32]. nevertheless, if we consider that studies show up to 70% of patients undergoing cabg with positive antibodies, it may not have other clinical findings of HIT and, the absence of antibody does not exclude the diagnosis of HIT, with possible further seroconversion [5]. moreover, in a recent study [33], the 4ts score is compared with the laboratory diagnosis of HIT and then the perspective of this score to be a clinical tool for screening is discussed, in order to identify the individual risk of each patient to have this disease. given these evidence, it is considered that this limitation does not invalidate the results.
CONCLUSION
Patients undergoing cardiac surgery who develop thrombocytopenia have high mortality rate and should be assessed regarding the diagnosis of HIT.
In the studied sample, the use of 4Ts score could discriminate higher incidence of thrombosis and, it was also learned that the higher the score, the higher hospital mortality.
REFERENCES
1. Stéphan F, Hollande J, Richard O, Cheffi A, Maier-Redelsperger M, Flahault A. Thrombocytopenia in a surgical ICU. Chest. 1999;115(5):1363-70.
2. Baughman RP, Lower EE, Flessa HC, Tollerud DJ. Thrombocytopenia in the intensive care unit. Chest. 1993;104(4):1243-7.
3. Warkentin TE, Sheppard JA, Horsewood P, Simpson PJ, Moore JC, Kelton JG. Impact of the patient population on the risk for heparin-induced thrombocytopenia. Blood. 2000;96(5):1703-8.
4. Lee DH, Warkentin TE. Frequency of heparin-induced thrombocytopenia. In: Warkentin TE, Greinacher A, eds. Heparin-induced thrombocytopenia. 3rd ed. New York:Marcel Deckker;2004. p.107-48.
5. Giffhorn H, Rampielli A, Bonatelli Filho L, Collaço J. Trombocitopenia adquirida e cirurgia cardíaca: relato de caso. Rev Bras Cir Cardiovasc. 2002;17(2):166-70.
6. Shantsila E, Lip GY, Chong BH. Heparin-induced thrombocytopenia. A contemporary clinical approach to diagnosis and management. Chest. 2009;135(6):1651-64.
7. Kerendi F, Thourani VH, Puskas JD, Kilgo PD, Osgood M, Guyton RA, et al. Impact of heparin-induced thrombocytopenia on postoperative outcomes after cardiac surgery. Ann Thorac Surg. 2007;84(5):1548-53.
8. Gettings EM, Brush KA, Van Cott EM, Hurford WE. Outcome of postoperative critically ill patients with heparin-induced thrombocytopenia: an observational retrospective case-control study. Crit Care. 2006;10(6):R161.
9. Selleng S, Selleng K, Wollert HG, Muellejans B, Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia in patients requiring prolonged intensive care unit treatment after cardiopulmonary bypass. J Thromb Haemost. 2008;6(3):428-35.
10. Oliveira GB, Crespo EM, Becker RC, Honeycutt EF, Abrams CS, Anstrom KJ, et al; Complications After Thrombocytopenia Caused by Heparin (CATCH) Registry Investigators. Incidence and prognostic significance of thrombocytopenia in patients treated with prolonged heparin therapy. Arch Intern Med. 2008;168(1):94-102.
11. Elalamy I, Le Gal G, Nachit-Ouinekh F, Lafuma A, Emery C, Le-Fur C, et al. Heparin-induced thrombocytopenia: an estimate of the average cost in the hospital setting in France. Clin Appl Thromb Hemost. 2009;15(4):428-34.
12. Smythe MA, Koerber JM, Fitzgerald M, Mattson JC. The financial impact of heparin-induced thrombocytopenia. Chest. 2008;134(3):568-73.
13. Hirsh J, Warkentin TE, Raschke R, Granger C, Ohman EM, Dalen JE. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinectics, dosing considerations, monitoring, efficacy, and safety. Chest. 1998;114(5 Suppl):489S-510S.
14. Warkentin TE, Heddle NM. Laboratory diagnosis of immune heparin-induced thrombocytopenia. Curr Hematol Rep. 2003;2(2):148-57.
15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818-29.
16. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter P, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793-800.
17. Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638-52.
18. Majerus PW, Broze GJ Jr, Miletich JP, et al. Anticoagulant, thrombolytic and antiplatelet drugs. In: Goodman LS, Gilman A, Rall TW, et al., eds. The pharmacological basis of therapeutics. 8th ed. New York:Pergamon Press;1990. p.1311.
19. Weismann RE, Tobin RW. Arterial embolism occurring during systemic heparin therapy. AMA Arch Surg. 1958;76(2):219-25.
20. Roberts B, Rosato FE, Rosato EF. Heparin: a cause of arterial emboli? Surgery. 1964;55:803-8.
21. Heijmans JH, Maessen JG, Roekaerts PM. Risk stratification for adverse outcome in cardiac surgery. Eur J Anaesthesiol. 2003;20(7):515-27.
22. Walls JT, Curtis JJ, Silver D, Boley TM. Heparin-induced thrombocytopenia in patients who undergo open heart surgery. Surgery. 1990;108(4):686-92.
23. Singer RL, Mannion JD, Bauer TL, Armenti FR, Edie RN. Complications from heparin-induced thrombocytopenia in patients undergoing cardiopulmonary bypass. Chest. 1993;104(5):1436-40.
24. Thong CL, Kam PCA. Heparin-induced thrombocytopenia. Curr Anaesth Crit Care. 2005;16(3):143-50.
25. Rice TW, Wheeler AP. Coagulopathy in critically ill patients: part 1: platelet disorders. Chest. 2009;136(6):1622-30.
26. Arepally GM, Ortel TL. Clinical practice. Heparin-induced thrombocytopenia. N Engl J Med. 2006;355(8):809-17.
27. Selleng S, Malowsky B, Strobel U, Wessel A, Ittermann T, Wollert HG, et al. Early-onset and persisting thrombocytopenia in post-cardiac surgery patients is rarely due to heparin-induced thrombocytopenia, even when antibody tests are positive. J Thromb Haemost. 2010;8(1):30-6.
28. Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, et al. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfracionated heparin. N Engl J Med. 1995;332(20):1330-5.
29. Ling E, Warkentin TE. Intraoperative heparin flushes and subsequent acute heparin-induced thrombocytopenia. Anesthesiology. 1998;89(6):1567-9.
30. Melo EI, Pereira MS, Cunha RS, Sá MPL, Mourão PAS. Controle da qualidade das preparações de heparina disponíveis no Brasil: implicações na cirurgia cardiovascular. Rev Bras Cir Cardiovasc. 2008;23(2):169-74.
31. Francis JL, Palmer GJ 3rd, Moroose R, Drexler A. Comparison of bovine and porcine heparin in heparin antibody formation after cardiac surgery. Ann Thorac Surg. 2003;75(1):17-22.
32. Gruel Y, Régina S, Pouplard C. Usefulness of pretest clinical score (4Ts) combined with immunoassay for the diagnosis of heparin-induced thrombocytopenia. Curr Opin Pulm Med. 2008;14(5):397-402.
33. Crowther MA, Cook DJ, Albert M, Williamson D, Meade M, Granton J, et al; Canadian Critical Care Trials Group. The 4Ts scoring system for heparin-induced thrombocytopenia in medical-surgical intensive care unit patients. J Crit Care. 2010;25(2):287-93.



 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license