Renato BRAULIO; Cláudio Léo GELAPE; Geraldo Brasileiro Filho; Maria da Consolação Vieira Moreira
DOI: 10.5935/1678-9741.20110026
ABSTRACT
A serious complication such as dissection of the left main coronary artery, with significant reduction in coronary blood flow by the true light, requires quick action. Therefore, the immediate choice of stent with appropriate length and size to treat the complication is necessary.RESUMO
Uma complicação grave, como a dissecção do tronco de coronária esquerda, com redução relevante do fluxo sanguíneo coronário pela luz verdadeira, requer ação rápida. Diante disso, a escolha imediata do stent no comprimento e calibre adequados para tratar a complicação se faz necessária.CASE STUDY
EDFS Patient, female, 60 years, original from Pernambuco. In January 2009, when she was home, she had an episode of severe chest pain accompanied by sweating and general malaise. She sought the local emergency care unit, where she was diagnosed with acute myocardial infarction (AMI) with supra-ST segment elevation. Also during the first visit the patient had an episode of cardiac arrest, being promptly revived, evolving without neurological deficit.
Transferred to a hospital of high complexity, after 12 hours of the onset of AMI, she underwent angioplasty of the LAD artery. During the procedure it was performed dissection of the left coronary artery trunk, thus, opting for stenting in the trunk.
The patient developed severe ischemic cardiomyopathy and heart failure class IV (NYHA), refractory to optimal medical treatment and without possibility of revascularization or geometric reconstruction of the left ventricle. She moved to Belo Horizonte-MG, she sought for the ambulatory of cardiac insufficiency of the UFMG, where she was then slated for heart transplantation at the HC-UFMG in August 2009. In April 2010, she underwent successful heart transplantation, progressing uneventfully and was discharged after 14 days of operation.
PRE-TRANSPLANTION ELECTROCARDIOGRAM
Sinus rhythm, HR: 72 bpm, anteroseptal inactivity.
PRE-TRANSPLANTION RADIOGRAPHY
Increased heart size and mild pulmonary congestion
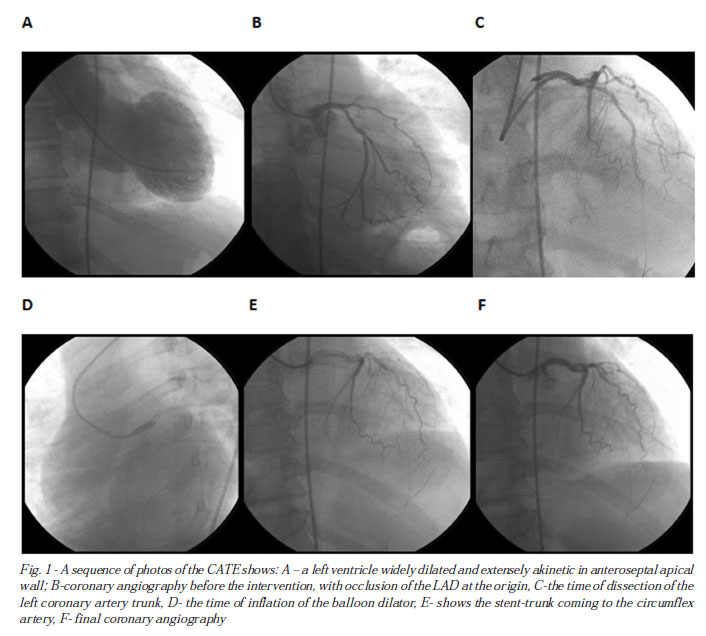
PRE-TRANSPLANTATION CORONARY ANGIOGRAPHY AND LEFT VENTRICULOGRAPHY (CATE)
Ostial occlusion of the circumflex artery and proximal subocclusion of left anterior descending artery, with extensive antero-apical akinesia to ventriculography.
PRE-TRANSPLANTION
ECODOPPLERCARDIOGRAM
Severe left ventricular dysfunction with apical aneurysm, anterior akinesia, apical, septal and severe mitral regurgitation, left ventricular ejection fraction: 19%, left ventricle during systole: 55 mm, left ventricle during diastole, 70 mm, left atrium 45 mm , pulmonary artery systolic pressure: 48 mmHg.
MYOCARDIAL SCINTILOGRAPHY WITH THALLIUM
Absence of myocardial viability in the anteroseptal and lateral regions.
OPERATION
Removal of the donor heart
Donor 35 years, male, 70 kg, the victim of traumatic brain injury after three days of internment without signs of infection, FiO2 40%, and using noradrenalin to 0.03 mcg / kg/min.
Median sternotomy, release and cava cerclage, systemic heparinization (4 mg / kg), drainage of the left atrium, aortic clamping, cardioplegia with Celsior ® ice solution at 4ºC, topical cardioplegia with cold saline solution, cardiectomia with preservation for transportation at 4ºC.
Implantation of the donor heart at the receiver
Median sternotomy and release of cava cerclage, systemic heparinization (4 mg/kg), entered into cardiopulmonary bypass (CPB) with cooling at 32ºC, aortic clamping, cardiectomia.
Implantation of the donor heart by the bicaval technique [3], maintaining cardioplegia with Celsior® ice solution every 20 minutes, following left atrial anastomosis, inferior vena cava, pulmonary artery, aorta, aortic declamping and anastomosis in the superior vena cava. Removal of CPB in the use of dobutamine and sodium nitroprusside uneventfully. Organ ischemia time of 98 minutes, CPB time and aortic clamping 90 and 73 minutes respectively.
The patient was extubated at the sixth hour after surgery, being discharged from the ICU after 03 days and discharged from hospital on the 14th day postoperatively, after the second endomyocardial biopsy. After 30 days of transplantation the patient was in functional class I during follow-up in the Transplant Clinic. She had complications as traumatic fracture of the calcaneus and was operated successfully.
Anathomic Pathologic Diagnosis
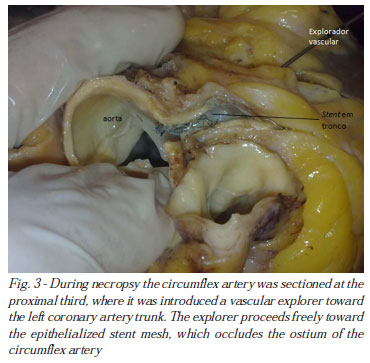
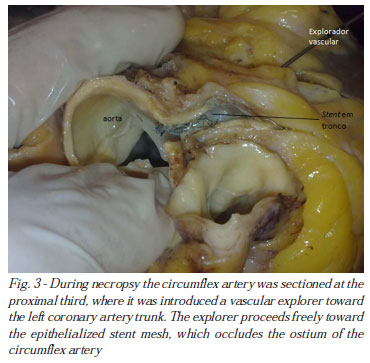
Macroscopic examination of the explanted heart showed that the stent implanted in the left coronary artery trunk (LCA) suffered partial extrusion into the lumen of the aorta and blocked the left circumflex artery (CX) (Figs. 1-3). The heart had a bulged edge and formed by the left ventricle. On sectioning, there was moderate dilatation of the left ventricular cavity, especially at the tip and the anteroseptal region. On the anterior wall of the left ventricle and the anterior interventricular septum it was found extensive old transmural healed myocardial infarction. In the trunk of the left coronary artery and in the anterior descending and circumflex arteries, atheromatous plaques of varied volume were seen, blocking up to about 80% of the vascular lumen, in the right coronary artery the atherosclerotic obstruction reached up to 20% of the vessel lumen.

DISCUSSION
The severe acute coronary dissection is the most common cause of acute occlusion after coronary angioplasty, occurring in 20 to 40% of cases [1,4]. The primary coronary angioplasty procedure is itself a rescue, always done on an emergency basis, where not always an optimal therapy is possible. A serious complication such as dissection of the left main coronary artery, with significant reduction in coronary blood flow by the true light, requires quick action by the intervention. Therefore, the immediate choice of stent length and size appropriate to treat the complication is necessary.
In our case, we observe a mismatch of the length of the stent in relation to the treated coronary trunk. The distal end of the stent was implanted after the ostium of the left anterior descending artery and the proximal end about 5 mm extrusa of the trunk into the aortic lumen. However, the mesh of the stent covered the ostium of the circumflex artery. Nevertheless, it is likely that initially a flow had occurred to the circumflex through the mesh of the stent. However, later it occurred the epithelialization of the mesh of the stent, leading to complete occlusion of the circumflex artery, as it can be seen in pathological examination of the explanted heart (Fig. 3). Therefore, one can expect that the opening of the circumflex artery by the technique of "kissing ballon", with the passage of a second guide through the mesh of the stent to access the circumflex, promoting the dilation balloon with two simultaneous trunk/DA and circumflex or even coronary artery bypass surgery could have alleviated the complication here.
Despite the scant literature on complications after stent implantation in cases of iatrogenic dissection of left coronary artery trunk, we believe that ischemic cardiomyopathy refractory may enter the list of complications of such treatment and should be considered and prevented during the procedures.
REFERENCES
1. Breda JR, Breda AS, Pires AC Operative treatment after iatrogenic left main dissection. Rev Bras Cir Cardiovasc. 2008;23(2):268-71. [MedLine] View article
2. McArdle H, Bhandari M, Kovac J Emergency coronary stenting of unprotected critical left main coronary artery stenosis in acute myocardial infarction and cardiogenic shock. Heart. 2003;89(9):24.
3. Chaccur P, Dinkhuysen JJ, Nina VJS, Abdulmassih NC, Arnoni AS, Souza LCB Transplante cardíaco ortotópico pela técnica bicaval. Rev Bras Cir Cardiovasc. 1997;12(2):145-52. View article
4. Salgueiro S, Silva AD, Tofano RJ, Costa VC, Pizarro K, Salman AA Percutaneous stent implantation for treating multivessel coronary disease in patients with and without involvement of the proximal segment of the anterior descending coronary artery. Arq Bras Cardiol. 2002;79(1):25-34. [MedLine]
Article receive on Monday, April 18, 2011
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license