Diego Felipe GaiaI; Aline CoutoII; João Roberto BredaIII; Carolina Baeta Neves Duarte FerreiraIV; Murilo Teixeira MacedoV; Marcus Vinícius GimenesV; Enio BuffoloVI; José Honório PalmaVII
DOI: 10.5935/1678-9741.20120062
ABSTRACT
OBJECTIVE: Aortic valve replacement for bioprosthesis dysfunction is a procedure involving considerable risk. In some cases, mortality is high and may contraindicate the procedure. Minimally invasive transcatheter aortic "valve-in-valve" implant appears to be an alternative, reducing morbidity and mortality. The objective is to evaluate aortic valve-in-valve procedure using Braile Inovare prosthesis.
METHODS: The Braile Inovare prosthesis, transcatheter, expandable balloon, was used in 14 cases. Average EuroSCORE was 42.9%. All patients had double aortic bioprosthesis dysfunction. Procedures were performed in a surgical hybrid environment under echocardiographic and fluoroscopic guidance. Using left minithoracotomy prostheses were implanted through the ventricular apex under high-frequency ventricular pacing. Serial clinical and echocardiographic controls were performed. Follow-up ranged 1-30 months.
RESULTS: Correct prosthetic deployment was obtained in all cases. There was no conversion. There was no operative mortality. The 30-day mortality was 14.3% (two cases). Ejection fraction increased significantly after the 7th postoperative day. Aortic gradient significantly reduced. The residual aortic regurgitation was not present. There were no vascular complications or complete atrioventricular block.
CONCLUSION: The transcatheter "valve-in-valve" procedure for bioprosthesis dysfunction is safe with low morbidity. This possibility may change prosthesis choice during the first aortic valve replacement, favoring bioprostheses.
RESUMO
INTRODUÇÃO: A reoperação para substituição de biopróteses aórticas com disfunção é procedimento que envolve considerável risco. Em alguns casos, a mortalidade é elevada e pode contraindicar o procedimento. O implante minimamente invasivo "valve-in-valve" transcateter de valva aórtica parece ser uma alternativa, reduzindo morbimortalidade. O objetivo deste estudo foi avaliar esses implantes utilizando a prótese Braile Inovare.
MÉTODOS: A prótese Braile Inovare, transcateter, balão expansível foi utilizada em 14 casos. Euroscore médio foi de 42,9%. Todos os pacientes eram portadores de dupla disfunção de bioprótese aórtica. Os procedimentos foram realizados em ambiente cirúrgico híbrido, sob controle ecocardiográfico e fluoroscópico. Por meio de minitoracotomia esquerda, as próteses foram implantadas através do ápice ventricular, sob estimulação ventricular de alta frequência. Foram realizados controles clínicos e ecocardiográficos seriados. O seguimento variou de 1 a 30 meses.
RESULTADOS: A correta liberação protética foi possível em todos os casos. Não ocorreu conversão. Não houve mortalidade operatória. A mortalidade em 30 dias foi de 14,3% (dois casos). A fração de ejeção apresentou aumento significativo após o 7º pós-operatório e o gradiente aórtico apresentou redução significativa. A insuficiência aórtica residual não esteve presente. Não ocorreu complicação vascular periférica ou bloqueio atrioventricular total.
CONCLUSÕES: O implante "valve-in-valve" de valva aórtica transcateter em biopróteses com disfunção é um procedimento seguro e com morbimortalidade baixa. Essa possibilidade poderá alterar a indicação de seleção de prótese no procedimento inicial, favorecendo próteses biológicas.
Descritores: Ponte cardiopulmonar. Estenose da valva aórtica. Cateterismo cardíaco.
EuroScore: European System for Cardiac Operative Risk Evaluation
STS: Score Society of Thoracic Surgeons score
INTRODUCTION
The degenerative aortic valve calcification is considered the most common cause of aortic stenosis in developed countries, the most frequent indication for aortic valve replacement [1]. Standard treatment consists of valve replacement with a prosthetic device (biological or mechanical), with operative mortality around 4% [2]. Despite these results, there are limitations. Bioprostheses have limited durability, evolving along with structural degeneration along with the follow-up and the mechanics have risks as mechanical dysfunction and thrombosis. In the event of valve replacement (reoperation), the risk is higher than expected for the first replacement. Furthermore, some patients exhibit even higher mortality due to various morbidities. The combination of risk factors may determine the contraindications of the procedure in 30% of cases [3].
Recently, several groups have proposed the use of transcatheter therapy in order to reduce morbidity and mortality associated with conventional intervention when applied to high-risk individuals [4,5]. The improvement of the technique has allowed its application more secure and with progressive improvement of outcomes [6-8]. Recently, several groups have proposed the use of transcatheter technology in degenerated bioprostheses, a procedure called "valve-in-valve", but the series is still limited and require confirmation as to its efficacy, safety and limitations [9].
In our environment, we developed a balloon-expandable prosthesis with encouraging initial results, including its use within degenerated bioprostheses [10,11].
The assessment of clinical results, safety and efficacy of the procedure performed with this new prosthesis within bioprosthesis dysfunction is the aim of this study.
METHODS
Patient Selection
Between June 2008 and December 2011, 14 patients from a single center underwent "valve-in-valve" transcatheter valve implantation being assessed prospectively, after signing an informed consent and Ethics Committee approval (CEP 1116/08).
Patients were selected by a multidisciplinary group. The selection of patients involved, in addition to multidisciplinary consultation and the inclusion and exclusion criteria, consideration of aspects such as high surgical risk, expectation, quality of life and assessment of biological fragility. The EuroSCORE and STS score risk scores were used in order to provide quantitative analysis of individual risk involved in the procedure.
Patients underwent clinical and laboratory tests, echocardiography, cineangiocoronariography and Doppler ultrasonography of iliac femoral and carotid systems.
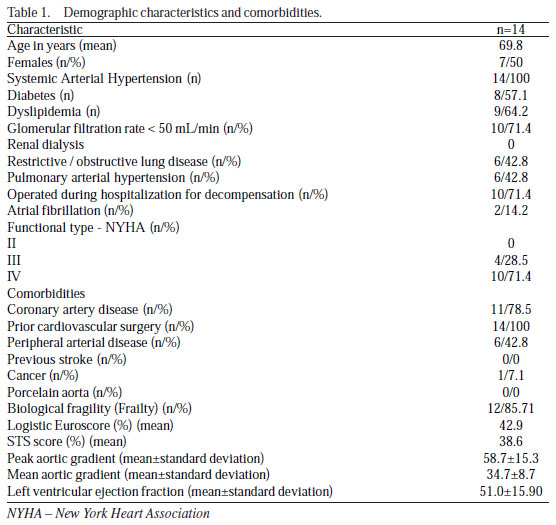
The inclusion and exclusion criteria are listed in another publication [11]. Patients with bioprosthesis measuring 19 mm in diameter were excluded from the indication due to high risk of residual gradients, given the extreme reduction of the valve area.Demographic characteristics and comorbidities of the patients are listed in Tables 1 and 2.

The prostheses presenting dysfunction were composed of a variety of manufacturers: 3 Porcine Braile Biomédica, 3 Medtronic Hancock, 2 Biocor and 6 unmarked.
Device and Procedure
The "valve-in-valve' aortic valve implantation was performed as previously described techniques [8,11]. All implants were performed with the aid of a surgical C-shaped arch (BV Pulsera, Philips Medical, The Netherlands), using radiolucent surgical table and dimensional Transesophageal echocardiography (C Envisor HD, Philips Medical, The Netherlands). Complete equipment for cardiopulmonary bypass was available in stand-by in all cases (Braile Biomédica, São José do Rio Preto, SP, Brazil). In all cases transcatheter balloon-expandable bioprosthesis was used (Braile Biomedica, São José do Rio Preto, SP, Brazil) in sizes 20 to 24 mm in diameter as the inner diameter of the bioprosthesis dysfunction, considering a size of about 10%.
Intraoperative transesophageal echocardiographic controls were performed after valve implantation and hemodynamic stabilization of the patient, in order to check the correct functioning of the prosthetic valve, as well as hemodynamic characteristics. Angiographic controls were performed only in the event of doubt on echocardiogram in order to avoid the use of iodinated contrast.
After the procedure, all patients were maintained on dual antiplatelet therapy protocol using aspirin and clopidogrel.
Follow-up and outcomes
Procedural success was defined as correct implant, satisfactory hemodynamic profile, the absence of significant valve or perivalvular leaks and no immediate major complications.
Patients were followed-up serially in the following postoperative: 1 day, 7 days, 30 days, 6 months, 12 months, 18 months and 24 months, with clinical and echocardiographic assessments.
The following outcomes were assessed: all-cause mortality (operative and 30 days post-discharge); major cardiovascular events, rehospitalization for prosthetic valve dysfunction or clinical deterioration; functional class; stroke, vascular complications, renal failure and bleeding. Outcomes were assessed according to the recommendations of the Valve Academic Research Consortium [12].
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 11. The confidence level of 0.05 was used as significant. The comparison between the means used the Friedman test after verification of normal distribution of values. The mean and standard error were used to express the analysis, unless otherwise specified. The Kaplan-Meier curve was used for survival analysis of appropriate outcomes.
RESULTS
Procedure
All cases were performed at the institution in a hybrid operating room. The successful valve implantation was performed in all cases. There were no conversions or prosthesis migrations.
The average time of implantation was 153.7 ± 42.1 minutes. The mean fluoroscopy time was 13.1 ± 7.5 minutes. The quantity of contrast medium used was 40.0 ml, while only the first four cases using contrast. No operative mortality occurred. There was no need to implant more than one valve in the same patient. Major vascular complication was not present. There was permanent pacemaker implantation. There was no severe or mild stroke. There was transient fall in platelet count in 5 cases.
We used the following device sizes: 2 of 20 mm, 7 of 22 mm and 5 of 24 mm.
The follow-up ranged from 1 to 33 months.
The surgical variables are listed in Table 2.
Mortality and hospital readmissions
Two patients died within 30 days. During the follow-up after hospital discharge, there was three deaths: a case of cardiogenic shock with normal functioning prosthesis, a case of acute myocardial infarction in patients with coronary artery disease not previously treatable of surgical or percutaneous treatment and one by right heart failure and severe pulmonary hypertension in a patient with sickle cell anemia (prosthesis normofunctioning) (Figure 1).

Evolution of functional class
The functional class improved significantly compared preoperatively at 1, 6 and 12 months (P <0.0001). A comparison of 1, 6 and 12 months did not show a statistically significant difference.
Echocardiographic assessment
The hemodynamic result assessed by echocardiography was satisfactory, with significant reduction of the peak gradient of 58.7 to 24.9 mmHg in the 1st postoperative day (P <0.001). The outcome showed that reducing the gradient was maintained in subsequent studies, with no statistically significant difference between the gradient obtained after implantation in the immediate postoperative period. The gradient also demonstrated a significant reduction of 34.7 mmHg to 12.8 mmHg on the first postoperative day (P <0.001). The outcome showed the maintenance of that reduction. The periprosthetic aortic insufficiency in the immediate postoperative period was not present.
Ventricular function measured by the left ventricular ejection fraction using the Simpson method showed statistically significant improvement from 51% to 55.6%, on the seventh day postoperatively (P <0.01), sustained during the follow-up.
The intraoperative variables are listed in Table 2.
DISCUSSION
The valve replacement surgery is the procedure of choice in patients with aortic valve stenosis or prosthetic valve dysfunction. In the majority of the population, intervention has low risk and is able to promote functional improvement and increase the survival rate when compared to clinical treatment [2.13]. Nevertheless, a progressively larger portion of that population has necessitated the replacement of dysfunctional prosthesis and, consequently, higher operative risk [14].
Within this context, the possibility of less invasive intervention through transcatheter implantation has become an attractive alternative. Several centers have published results consistent with progressive reduction of complications and mortality in selected patients [7,9,11,15].
In the selected cases for implantation on a failed bioprosthesis, the results are even more encouraging, since the risks of complications and possible periprosthetic leaks are substantially smaller than the implant when compared to a native valve, making it even a more attractive alternative [9].
When compared to the implant on native prosthesis, it is noteworthy that prior identification of prosthesis dysfunction may be of extreme importance, since the same nominal diameters vary by manufacturer and landmarks chosen in the measurement. Moreover, radiological identification is also quite variable, and may lead to difficulty in precise location of the best implant site and the prosthetic ring. Some devices also require radiopaque markers, making the implant more dependent on the use of contrast media and transesophageal echocardiography. In case of lack of prior reliable information or unfavorable echocardiographic windows, CT may play an important role in measuring the annulus and collaborate to select the correct size of the device to be implanted.
Hospital mortality of the procedure is quite variable in the literature, but the groups, most often, are not comparable. The observed risk is lower than predicted by risk scores, although there are several questions about its validity [16].
The overall mortality compared to the expected risk scores demonstrates, again, that procedure is able to provide additional benefits in terms of survival. Survival after hospital discharge is also significant and causes of mortality in evolution were not related to the prosthetic device. Likewise, there was no structural degeneration of implanted prostheses, although this segment is still short for their definitive assessment [5].
The mean age of the study population is lower than that found in other studies, however, it is noteworthy that given the prevalence of rheumatic fever in the Brazilian population the average age in the realization of the first intervention is less. This fact explains why younger patients had already undergone multiple prior surgeries, raising their operative risk and justifying their inclusion in the study.
Complications occurred previously were not found in this sample [17]. Failure to proper occlusion of the left ventricular apex was not present. Some factors contribute to this finding, as the learning curve and the presence of adhesions that facilitate the support points and help the apical occlusion.
There were no cases of need for renal replacement therapy with hemodialysis, despite the presence of high glomerular filtration rate below 50%. Possibly, the low use of iodinated contrast collaborated to preserve renal function.
In all cases, we used the apical via to the transcatheter implant. The use of apical via, although more invasive, has additional advantages: 1. The prosthesis positioning is easier, given the proximity of the ventricular insertion point and aortic ring 2. The crossing of the failed prosthesis using guidewire and catheter insertion systems is easier, due to its ventricular aspect, due to the position of the valve leaflets; 3. The manipulation of the aortic arch is smaller, reducing the possibility of stroke 4. Navigation through the peripheral arterial system with the prosthesis is unnecessary, possibly contributing to the reduction of vascular complications.
Moreover, the presence of minithoracotomy certainly contributes to some degree of chest pain and transient deterioration of ventilatory capacity of these patients, contributing to the occurrence of comorbidities related to such dysfunction.
Structural valve deterioration still is a parameter difficult to assess and compare in the literature, due to the short follow-up period, and the small range of prostheses available. It is worrying that the fact of needing valve leaflets by balloon compression and expansion can theoretically cause premature structural deterioration thereof. [18] In our series, there was no deterioration of leaflets valve function during follow-up.
The atrioventricular block is a complication often described, and may reach one third of patients, especially with CoreValve [19]. Balloon-expandable prostheses, such as the Edwards Sapien and Inovare, had rates of need for permanent cardiac pacing at about 4.5% [7]. The presence of a prosthetic ring previously implanted probably protects the cardiac conduction system and, therefore further compression of complete atrioventricular block.
The need for conversion to conventional procedure, cardiopulmonary support and total valve replacement is reported as being around 3.5% [20]. In the present sample conversions did not occur. When compared to the implant on the native valve, it is expected an easier and safer procedure for many reasons: the suitable valve diameter is more easily found, since in most cases the diameter of the ring failed prosthesis is known or easily measured by imaging, such as computed tomography, allowing better selection of appropriate valve size and the presence of prosthetic dysfunction facilitates the identification of the correct position to release the device, reducing the possibility of implant embolization and also the risk of obstruction of the coronary ostia is also lower.
The assessment and echocardiographic follow-up of patients undergoing transcatheter therapy is of paramount importance when comparing different devices and conventional aortic valve replacement. The performance and durability of these new prostheses require constant assessment, because of the extensive differences in valve design, and its mode of implant fixation mechanism. There are no long-term data on these variables. The hemodynamic profile of these prostheses is superior to the traditional models, whether support-mounted or stentless. The absence of large supporting structures contributes to the superiority, providing significant gain in effective orifice. Comparisons between the hemodynamic performance and evolution of improvement in ventricular function are markedly superior in patients undergoing transcatheter implantation compared to the usual intervention [21,22]. In "valve-in-valve" cases there is significant concern about the reduction in the effective valve orifice, this fact is noted by the lower transvalvular aortic gradient reduction when compared to implant on native valves [11]. Thus, the implant within bioprosthesis with diameters less than 21 mm is questionable, as well as implantation of a second transcatheter valve. Ongoing and unpublished studies intend to clarify the theoretical limits of "valve-in-valve" implant.
The transvalvular gradients after implantation decreased compared with the preoperative period and remained low during follow-up, demonstrating a favorable hemodynamic profile of this device. This maintenance is similar to that found in other commercially available prostheses [22].
Ventricular function improves significantly early and during the follow-up. On the seventh postoperative day, we should observe a significant increase. The rapid improvement may partly explain the differences in mortality observed between conventional and transcatheter procedure. No use of cardiopulmonary bypass and aortic clamping under cardioplegic protection and the presence of a lower afterload generated by transcatheter prostheses are possible causes [21,22].
The study has limitations such as sample size and follow-up time. Identifying individuals with greater benefit with this strategy is only possible with larger numbers of patients and long-term observational period. The randomization facing medical treatment and open replacement may confirm the findings.
CONCLUSION
"Valve-in-valve" transcatheter treatment using the Inovare prosthesis shows results comparable to the literature using other prostheses, with the advantage of greater diversification in size and consequent lower gradients. It is able to provide benefits to cardiac structural and functional improvement. It is mandatory to further follow-up aiming at measuring benefits, complications and improving selection criteria.
The conventional intervention remains the gold standard for low risk patients, but this new strategy can be recommended for selected groups with contraindications to the traditional procedure.
REFERENCES
1. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999;341(3):142-7. [MedLine]
2. Edwards FH, Peterson ED, Coombs LP, DeLong ER, Jamieson WR, Shroyer ALW, et al. Prediction of operative mortality after valve replacement surgery. J Am Coll Cardiol. 2001;37(3):885-92. [MedLine]
3. Iung B, Cachier A, Baron G, Messika-Zeitoun D, Delahaye F, Tornos P, et al. Decision-making in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26(24):2714-20. [MedLine]
4. Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106(24):3006-8. [MedLine]
5. Walther T, Falk V, Kempfert J, Borger MA, Fassl J, Chu MW, et al. Transapical minimally invasive aortic valve implantation; the initial 50 patients. Eur J Cardiothorac Surg. 2008;33(6):983-8. [MedLine]
6. Webb JG, Altwegg L, Boone RH, Cheung A, Ye J, Lichtenstein S, et al. Transcatheter aortic valve implantation: impact on clinical and valve-related outcomes. Circulation. 2009;119(23):3009-16. [MedLine]
7. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597-607. [MedLine]
8. Gaia DF, Palma JH, de Souza JA, Ferreira CB, Macedo MT, Gimenes MV, et al. Transapical mitral valve-in-valve implant: an alternative for high risk and multiple reoperative rheumatic patients. Int J Cardiol. 2012;154(1):e6-7.
9. Webb JG, Wood DA, Ye J, Gurvitch R, Masson JB, Rodés-Cabau J, et al. Transcatheter valve-in-valve implantation for failed bioprosthetic heart valves. Circulation. 2010;121(16):1848-57. [MedLine]
10. Gaia DF, Palma JH, Souza JA, Guilhen JC, Telis A, Fischer CH, et al. Off-pump transapical balloon-expandable aortic valve endoprosthesis implantation. Rev Bras Cir Cardiovasc. 2009;24(2):233-8. [MedLine] View article
11. Gaia DF, Palma JH, Ferreira CB, Souza JA, Agreli G, Guilhen JC, et al. Transapical aortic valve implantation: results of a Brazilian prosthesis. Rev Bras Cir Cardiovasc. 2010;25(3):293-302. [MedLine] View article
12. Leon MB, Piazza N, Nikolsky E, Blackstone EH, Cutlip DE, Kappetein AP, et al. Standardized endpoint definitions for transcatheter aortic valve implantation clinical trials: a consensus report from the Valve Academic Research Consortium. Eur Heart J. 2011;32(2):205-17. [MedLine]
13. Grossi EA, Schwartz CF, Yu PJ, Jorde UP, Crooke GA, Grau JB, et al. High-risk aortic valve replacement: are the outcomes as bad as predicted? Ann Thorac Surg. 2008;85(1):102-6.
14. Gummert JF, Funkat AK, Beckmann A, Ernst M, Hekmat K, Beyersdorf F, et al. Cardiac surgery in Germany during 2010: a report on behalf of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg. 2011;59(5):259-67. [MedLine]
15. Gaia DF, Palma JH, de Souza JA, Buffolo E. Tricuspid transcatheter valve-in-valve: an alternative for high-risk patients. Eur J Cardiothorac Surg. 2012;41(3):696-8. [MedLine]
16. Yan TD, Cao C, Martens-Nielsen J, Padang R, Ng M, Vallely MP, et al. Transcatheter aortic valve implantation for highrisk patients with severe aortic stenosis: A systematic review. J Thorac Cardiovasc Surg. 2010;139(6):1519-28. [MedLine]
17. Gaia DF, Palma JH, Ferreira CB, Souza JA, Agreli G, Guilhen JC, et al. Transapical aortic valve implantation: results of a Brazilian prosthesis. Rev Bras Cir Cardiovasc. 2010;25(3):293-302. [MedLine] View article
18. de Buhr W, Pfeifer S, Slotta-Huspenina J, Wintermantel E, Lutter G, Goetz WA. Impairment of pericardial leaflet structure from balloon-expanded valved stents. J Thorac Cardiovasc Surg. 2012;143(6):1417-21. [MedLine]
19. Fraccaro C, Buja G, Tarantini G, Gasparetto V, Leoni L, Razzolini R, et al. Incidence, predictors, and outcome of conduction disorders after transcatheter self-expandable aortic valve implantation. Am J Cardiol. 2011;107(5):747-54. [MedLine]
20. Thomas M, Schymik G, Walther T, Himbert D, Lefèvre T, Treede H, et al. Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: A European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation. 2010;122(1):62-9. [MedLine]
21. Zhao Y, Lindqvist P, Nilsson J, Holmgren A, Näslund U, Henein MY. Trans-catheter aortic valve implantation: early recovery of left and preservation of right ventricular function. Interact Cardiovasc Thorac Surg. 2011;12(1):35-9. [MedLine]
22. Clavel MA, Webb JG, Pibarot P, Altwegg L, Dumont E, Thompson C, et al. Comparison of the hemodynamic performance of percutaneous and surgical bioprostheses for the treatment of severe aortic stenosis. J Am Coll Cardiol. 2009;53(20):1883-91. [MedLine]
Article receive on Tuesday, May 8, 2012
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license