Patrick Bastos MetzgerI; Fabio Henrique RossiII; Samuel Martins MoreiraIII; Mário IssaIV; Nilo Mitsuru IzukawaV; Jarbas J. DinkhuysenVI; Domingos Spina NetoVII; Antônio Massamitsu KambaraVIII
DOI: 10.5935/1678-9741.20140056
ABSTRACT
INTRODUCTION: The management of thoracic aortic disease involving the ascending aorta, aortic arch and descending thoracic aorta are technically challenging and is an area in constant development and innovation.
OBJECTIVE: To analyze early and midterm results of hybrid treatment of arch aortic disease.
METHODS: Retrospective study of procedures performed from January 2010 to December 2012. The end points were the technical success, therapeutic success, morbidity and mortality, neurologic outcomes, the rate of endoleaks and reinterventions.
RESULTS: A total of 95 patients treated for thoracic aortic diseases in this period, 18 underwent hybrid treatment and entered in this study. The average ages were 62.3 years. The male was present in 66.7%. The technical and therapeutic success was 94.5% e 83.3%. The perioperative mortality rate of 11.1%. There is any death during one-year follow-up. The reoperation rates were 16.6% due 2 cases of endoleak Ia and one case of endoleak II. There is any occlusion of anatomic or extra anatomic bypass during follow up.
CONCLUSION: In our study, the hybrid treatment of aortic arch disease proved to be a feasible alternative of conventional surgery. The therapeutic success rates and re- interventions obtained demonstrate the necessity of thorough clinical follow-up of these patients in a long time.
RESUMO
INTRODUÇÃO: O manejo das doenças da aorta torácica que envolvem a aorta ascendente, arco aórtico e aorta torácica descendente constituem um desafio técnico e é uma área em constante desenvolvimento e inovação.
OBJETIVO: Analisar os resultados iniciais e a médio prazo do tratamento híbrido das doenças do arco aórtico.
MÉTODOS: Estudo retrospectivo de procedimentos realizados no período de janeiro de 2010 a dezembro de 2012, em que foram analisados o sucesso técnico e terapêutico, a morbimortalidade, os desfechos neurológicos, a taxa de vazamentos e de reintervenções.
RESULTADOS: Em um total de 95 pacientes tratados por doenças da aorta torácica no período, 18 realizaram o tratamento híbrido e adentraram neste estudo. A idade média foi de 62,3 anos. O sexo masculino esteve presente em 66,7%. O sucesso técnico e terapêutico foi de 94,5% e 83,3%, respectivamente. A mortalidade perioperatória foi de 11,1%. Não houve óbito durante o acompanhamento de 1 ano. A taxa de reintervenção foi de 16,6%, devido a 2 casos de endoleak tipo Ia e um caso de endoleak tipo 2. Não foi observada oclusão dos enxertos anatômicos ou extra-anatômicos durante o período de seguimento.
CONCLUSÃO: O tratamento híbrido das doenças do arco aórtico demonstrou ser uma alternativa viável à cirurgia convencional. As taxas de sucesso terapêutico e de reintervenções demonstram a necessidade do seguimento clínico rigoroso desses pacientes a longo prazo.
INTRODUCTION
The management of patients with thoracic aortic diseases involving the ascending aorta, aortic arch and descending thoracic aorta are a technical challenge and is an area in constant development and innovation[1,2]. Traditionally, the total surgical repair of the aortic arch demand a period of deep hypothermic circulatory arrest, which can cause high rates of perioperative morbimortality[1-3].
The supra-aortic trunk derivations followed by the endovascular aortic repair is a less invasive alternative for the treatment of this serious condition, having been reported in several clinical trials, systematic reviews and recent meta-analyzes[3-5].
The total endovascular repair of the aortic arch has been a promising method in the last two decades, however, there is information divergence in the literature on the safety of the short-and-medium-term technique, patient selection criteria, in addition, little is known about the material durability and the long-term method[5-8].
The data available in the literature of different types of treatment are the result of small case series with heterogeneous samples and limited follow-up of patients[9]. Therefore, the ideal method for the treatment of aortic arch disease is still a matter of intense debate.
The objective of this study is to analyze the results in the short and medium term of a consecutive series of patients undergoing hybrid treatment of the aortic arch disease having as the outcomes studied the technical and therapeutic success, perioperative morbimortality and 1 year after the treatment, neurological outcomes after 30 days, the leak rate and reintervention during the follow-up period.
METHODS
Type of study
This is a retrospective, longitudinal and observational study carried out in two reference centers for cardiovascular diseases, from January 2010 to December 2012, with a total of 18 patients undergoing hybrid repair of aortic arch disease.
Inclusion and exclusion criteria
The study included patients of both sexes, with or without thoracic symptoms, with indications for aortic correction by:
1. Thoracic aortic aneurysms with a diameter greater than 60 mm or acute complicated Stanford type B aortic dissections (AAD), with inadequate proximal anchor zones (length <2 cm and/or presence of thrombus or calcified plaques greater than 50% of the circumference of the proximal colon)
2. Aortic arch pseudoaneurysm.
3. Penetrating ulcers of the aortic arch and thoracic aorta with a diameter of more than 2 cm and a depth of 1 cm without proximal anchor zones.
4. True aneurysms of the aortic arch (TAAA).
5. Chronic type A aortic dissection.
The study excluded patients with: proximal aortic neck fixation with extention greater than 20 mm, diameter of external iliac arteries smaller than 7 mm, serum creatinine greater than 2.0 mg/dl or creatinine clearance less than 30 ml/min.
Patients who underwent endovascular repair of thoracic aortic aneurysm and those who did not undergo the supra-aortic trunk revascularization were excluded from the present study.
The evaluation of cardiac and/or anesthetic risk was not considered in the inclusion or exclusion.
The treatment planning was performed with angiotomography in all patients, and the pre-operative arteriogram was an optinal diagnostic method. All scans were reconstructed in OSIRIX® MD software 3D mode (three-dimensional) and MPR mode (multiplanar reconstruction), and then the diameters, angles and extensions of the proximal aortic neck were obtained (Figure 1).
Surgical technique
The extension of the supra-aortic trunks revascularization was scheduled after the angiotomography evaluation of proximal anchoring zones and stratified using the Ishimaru & Mitchell classification[10] (Figure 2):
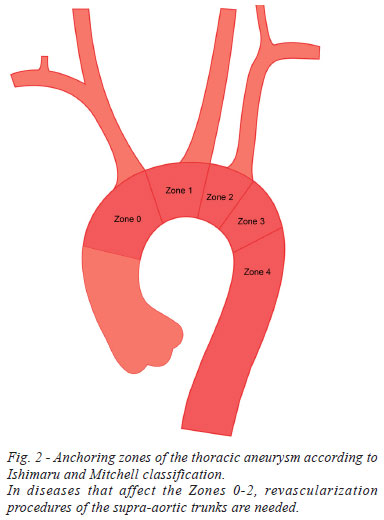
Zone 0: Revascularization of 3 or 4 supra-aortic vessels with median sternotomy (Figure 3A).
Zone 1: Carotid-carotid graft with retropharyngeal tunneling or anterior to the trachea associated with the subclavian artery revascularization by transposition or carotid-subclavian graft (Figure 3B).
Zone 2: Subclavian artery revascularization byb transposition or carotid-subclavian graft (Figure 3C).
Endovascular technique
All procedures were performed in the catheterization laboratory of the Endovascular Intervention Center (CIEV) of Dante Pazzanese Carfiology Institute and Salvalus Hospital, by the same group of vascular, cardiovascular surgeons and interventional radiologists.
The patients were treated under inhalation general anesthesia. Antibiotic prophylaxis was performed with 1.5 g of cefuroxime at the anaesthetic induction time. The approach was preferably carried out through the common femoral artery by unilateral open surgical dissection. As it was unsuccessful, we decided to approach the external iliac artery using a retroperitoneal approach.
Radiographic control was performed with Siemens® Artis Flat Panel device or in hybrid room with Siemens® Artis zeego Hybrid device. The devices used were: Valiant® (Medtronic Inc, Santa Rosa, Calif), Zenith TX2® (Cook, Bloomington, Ind), Tag® (WL Gore & Assoc, Flagstaff, Ariz), Relay® (Bolton Medical, Sunrise, Fla). The diameters of the stents ranged from 10% to 20% depending on the aortic disease that has to be treated. In cases of true aneurysms, we used an oversize of 20% and in the case of dissection, 10% to 15%.
The drainage of cerebrospinal fluid was carried out in selected cases depending on the extent of coverage of the aorta or presence of previous aortic surgeries.
In patients where the prostheses were implanted in Zone 0, tachycardia induced by temporary pacemaker was used. In cases of implantation in zone 1 and 2, permissive hypotension was used for accurate endoprosthesis deployment.
Intraoperative angiography was performed in all patients. The immediate postoperative period was performed in an intensive care unit in all cases.
Postoperative follow-up
Patients were followed up with outpatient evaluation on the 15th, 30th, 180th, and 360th days after the correction. After the first year, the consultations were held annually. The control with angiotomography was performed on the 30th and 360th days of the follow-up period. Ultrasound - Doppler (USG-D) was performed on the 30th and 180th days and annually in order to evaluate the patency of the supra-aortic grafts.
Outcomes and definitions
The primary outcome analyzed were defined as follows:
1 - Technical Success: When the derivation of the supra-aortic trunks was carried out in a previously planned manner; the objective to release the stent in the affected area has been achieved, even in the presence of leaks or other events that could adversely influence the evolution of aortic disease.
2 - Therapeutic Success: The stent deployment occurred without type I and/or III endoleak, or other complications that would affect the favorable development of aortic disease, preserving the patency of the supra-aortic trunk revascularizations.
3 - Perioperative Mortality: Number of deaths registered within the first 30 days after the procedure.
4 - Neurological morbidity in the first 30 days: ischemic cerebrovascular accident (ICVA) and paraplegia secondary to spinal cord ischemia.
5 - Mortality during the one-year-follow-up period.
RESULTS
In the period from January 2010 to December 2012, 95 endovascular correction of thoracic aortic diseases were performed, in which 18 patients underwent hybrid fix consecutively. The demographic characteristics, comorbidities and treatment indications are described in Table 1. The mean age was 62.3±8.3 years, with prevalence of males. The patients were asymptomatic in 13 cases (72.2%), and they were diagnosed in routine examinations findings. Hypertension was present in all patients. Among the present comorbidities, we found a high incidence of chronic obstructive pulmonary disease (COPD) (44.4%) and ischemic heart disease (27.8%). We also observed that 2 patients underwent previous correction of aortic aneurysm (11.1%) and 1 underwent endovascular repair of abdominal aortic aneurysm. (Table 1) Most of the indications for hybrid treatment were: true aneurysms of the aortic arch and descending thoracic aorta with colon anchoring <2 cm or unfavorable (Table 1).

Most patients were electively treated (72.2%), with the hybrid treatment staged in two phases. Five patients with type A dissection or complicated acute B dissection underwent emergency surgery with surgical and endovascular treatment at the same time. Inhalation general anesthesia was used in all cases with selective cerebrospinal fluid drainage.
The techniques used for the supra-aortic trunk revascularizations are described in Table 2. Eight anatomical grafts were performed (total revascularization of the aortic arch) and 10 extra-anatomic grafts (left-right carotid-carotid grafts and/or grafts or left carotid-subclavian transposition). All anatomical grafts were made with bifurcated and/or straight Dacron prosthesis.The extra-anatomic bridges were performed using PTFE annealed 6 or 8 with retropharyngeal tunneling in 2 cases and 1 case of tunneling anterior to the trachea.

Regarding the left subclavian carotid bridges, 7 transpositions of subclavian artery and 3 carotid-subclavian grafts. One of the patients have had previous correction of the ascending aorta, thus, we performed a graft of the ascending aorta-brachiocephalic trunk associated with carotid-carotid graft, and then, a vascular plug implantation in the origin of the brachiocephalic trunk and endovascular aortic repair with stent implantation in Zone 0. In this case, intentional occlusion of the left subclavian artery was performed after confirmation of patency and dominance of the right vertebral artery (Figure 3). Venous, lymphatic or neurological lesions were not observed during the intra-and postoperative period. During the one-year-follow-up period, there were no occlusions or hemodynamically significant stenoses in the anatomical or extra-anatomic grafts (Figures 4 and 5).
The revascularizations requiring the segment exchange of the ascending aorta were performed with total cardiac arrest and cardiopulmonary bypass, as in cases where only the supra-aortic revascularization was used, the proximal anastomosis was performed by partial aortic clamping without interruption flow. The cervical anastomoses were marked with radiopaque material in order to facilitate the endoprosthesis implantation. All aortic accesses were performed by conventional median sternotomy. Cervical access via supraclavicular incision and/or unilateral or bilateral anterior cervical were used depending on the desired type of supra-aortic revascularization.
The technical success was achieved in 94.5%, in other words, we were able to perform the programmed supra-aortic graft in 17 patients and, insert the stent into the desired position.
Therapeutic success was 83.3%, in other words, the prosthesis was inserted in 15 patients without leaks or other complications that would jeopardize the favorable evolution of the intervention. The therapeutic failure causes were the type I leak in two cases and one death in the intraoperative period during a correction of Stanford type A dissection, which evolved with retrograde dissection and aortic rupture with cardiac tamponade.
The in-hospital postoperative complication rate was 27.7%, as follows: two ischemic neurological injuries (11.1%), two cases of pulmonary complications (11.1%) and one case of acute renal failure (5, 5%) (Table 3).

The perioperative mortality was 11.1%. The two deaths occurred due to retrograde type A dissection: one by rupture and acute cardiac tamponade during the endovascular treatment and another by left coronary trunk dissection and acute myocardial infarction on the 8th day after surgery (Table 4). There were no deaths after the 30-day-follow-up period.

The primary leak rate was 16.6%, with the type I endoleak in two cases and type II in one case. No cases of type III leaks and stent migration during follow-up were observed. The reintervention rate after one year was 16.7% due to the treatment of type I and II leaks in a satisfactory manner (Table 4). The annual survival during our follow-up period was 89.9%.
The stent devices used were: in seven cases (38.9%) Zenith TX2® (Cook Medical, Bloomington, INC, USA), in six cases (33.3%) Tag® (Gore Medical, Flagstaff, AZ, USA) in three cases (16.6%) Valiant® (Medtronic, Minneapolis, MN, USA), and in two cases (11.1%) Relay® (Bolton Medical, Sunrise, Fla). We used a total of 21 stents.
The average time of endovascular procedure was 65 min (ranging from 48 to 151 minutes), the average time of the supra-aortic trunk revascularization was 196 minutes and the mean hospital stay was 9.7 days, with a 10-day variation. The mean follow-up time was 13 months (5-22 months).
DISCUSSION
The improvement of endovascular techniques and the association to surgical revascularization of the supra-aortic trunks allowed its application in aortic arch diseases, territory in which the conventional surgical treatment can bring high morbimortality rates[11]. Systematic reviews and recent clinical studies have confirmed the benefits of endovascular method over conventional surgery in this aortic segment[1-3,7,11-13]. A suitable anchoring zone in which there is at least 2 cm of healthy aortic extension is required for proper stent implantation, thereby preventing type I endoleak and maintaining the prosthesis durability for a long period[14].
For patients with unfavorable proximal colon, the supra-aortic trunk revascularizations, with the advanced endovascular aortic device for healthy aortic zones, make the treatment of this disease feasible, avoiding the conventional surgical procedure that requires circulatory arrest and deep hypothermia. The mortality of the conventional surgical procedure on the aortic arch varies 0.9 9.3% even in centers with a large number of surgery[3,15,16]. However, according to data from the National Inpatient Sample Database and Medicare Provider Analysis and Reviewer, that better reflect the global reality, mortality rates range from 15 to 20%[17-20]. Despite the invasiveness of the hybrid technique, its degree of morbidity can be minimized by using shorter aortic clamping or partial clamping techniques when you need to advance the prosthesis to Zone 0. In cases where a suitable landing colon can be obtained in Zones 1 and 2, the procedures staged without aortic clamping with the use of extra-anatomic grafts should be used[2,3].
We obtained a technical success rate of 94.5% and a therapeutic success rate. The technical success rate was influenced by intraoperative death, while the therapeutic success rate was influenced by the presence of type IA endoleaks, generating a primary leak rate of 16.6%. Both type IA leaks were treated with the advancement of a second larger diameter endoprosthesis with the leak fully sealed, whereas the type II leak through the subclavian artery was embolized using a spring, which generated a reintervention rate of 16.6%. Moulakakis et al.[1] reported a technical success rate of 92.8%, with a similar leak rate of 16.6%, which were mostly type I endoleaks. The authors explain this data due to the presence of retrograde type A dissection in 4.5% of their patients with the advancement of the stent to Zone 0[1].
Currently, the late results of the hybrid treatment of the aortic arch are not well known, with the most studies reporting a follow-up period of 15 to 18 months[6,21]. These data are extremely scarce and heterogeneous when the endoleaks are specifically evaluated. This rate varies in the literature from 0 to 15%, and the long-term data leaks are virtually absent[4,8,21]. Czerny et al.[4] in a recent study of transcontinental record data including 66 patients with complete revascularization of the aortic arch and a mean follow-up period of 25 months, only one late endoleak type IB and a 5-year survival of 96% was observed by the researchers. On the other hand, Vallejo et al.[6] in a series of 38 hybrid repair of the aortic arch, with a mean follow-up perid of 28 months, found four type I and two type II endoleaks[6]. Bavaria et al.[8] in a 30-month-follow-up period, did not observe the presence of type I or III leaks. In our study, we observed the presence of late type I, II and III leaks during the mean follow-up period of 13 months.
The population of our study showed high risk for conventional surgery due to the high prevalence of chronic obstructive pulmonary disease (50%) and ischemic heart disease (38.9%), and 5 of these patients were treated on an emergency basis due to complicated acute type A a or type B dissections, so our mortality rate in a 30-day-follow-up period was 11.1%. One patient died during the intraoperative period due to progression of retrograde type A dissection with aortic rupture and cardiac tamponade and another patient died on the 8th postoperative day due to the progression of type A dissection with retrograde left coronary trunk involvement and acute myocardial infarction. Brazilian authors reported a mortality rate of 16.7% in the perioperative period using the same technique[2]. A recent meta-analysis published in 2013, with 956 patients analyzed, obtained a perioperative mortality rate of 11.9%[1]. However, smaller case series have been published with mortality rates ranging between 3-6%[3,11].
The neurological injury rates in the literature range from 4% to 12%[11]. When we separate ICVA of the spinal cord from permanent paraplegia, we observed rates of 7.6% and 3.6% respectively, in the meta-analytic study by Moulakakis et al.[1]. In our region, we observed an ICVA rate of 5.5%. This occurred during the advancement of the stent to Zone 0. The occurrence of neurological outcome is directly related to the quality of the native aorta, with the unfavorable characteristics the presence of plaques and thrombi in the aortic segment[22]. Low ICVA rate found by Shirakawa et al.[11] in their clinical study with 40 patients and a follow-up of 15.5 months, is justified by the author due to careful preoperative selection of patients with angiotomography, evaluating the endoprosthesis implantation conditions in the ascending aorta. When a healthy aorta was found, the hybrid treatment was performed[11].
We had a case of spinal cord ischemia in a patient who previously had an open repair of the ascending aorta and prior endovascular repair of infrarenal abdominal aortic aneurysm. This patient had paraplegia signals on the 3rd postoperative day, therefore immediate fluid drainage was performed, however, this individual remained with permanent paraplegia as a sequel. Spinal cord ischemia is directly related to aortic coverage area and the aortic clamping time[1,3,23], thus, spinal cord ischemia rates in hybrid procedures are lower when compared to the open aortic corrections, since the aortic coverage area in hybrid procedures is smaller, as well as the clamping time. In this patient, the area of previous aortic management to the hybrid procedure favored this complication.
As for the postoperative complications, we highlight the low incidence of pulmonary complications (11.1%). Two patients had prolonged weaning and associated pulmonary infection being treated in the intensive care unit for a long period, but they evolved satisfactorily. The main clinical morbidity in the postoperative period of open and hybrid treatment of thoracic aortic diseases are pulmonary and cardiac complications. The rates of these complications were 19.7% and 6%, respectively, in the meta-analysis published in 2013[1]. In our study, we had one death due to acute myocardial infarction caused by retrograde dissection with left main coronary artery involvement. Despite the large number of COPD patients in our study, the low rate of pulmonary complications is explained due to strict stratification and preoperative clinical training, as well as intensive care dedicated to adequate cardiopulmonary rehabilitation.
The retrograde type A dissection is a complication described in the open and endovascular repair of the native ascending aorta[1,7,21]. When assessing the clinical studies for the presence of this complication, it is observed that the data are published in relation to all treated sample, with an absolute rate of 3.8% in the most recent meta-analysis published; however, when observing only the native ascending aorta at risk, we obtain higher rates of this complication. In the study published by Andersen et al.[7], a similar incidence of 3.4% is reported in a series of 87 patients with hybrid aortic arch repair. However, the authors report that the real rate should be 11.1% (3 of 27 cases) when they includ only patients with native ascending aorta at risk of this complication[3,7]. We had two cases of retrograde type A dissection in 16 native ascending aorta (12.5%).
New techniques with the full endovascular management of aortic arch aneurysms using branched and fenestrated stents are under development. The first clinical study is being conducted and, therefore, little is known about the medium and long term results of this technique[24]. Endovascular procedures using the Snorkel and Chaminé techniques, although feasible, they expose the patient to type I endoleak and retrograde type A dissection[25].
Study limitations
Due to the small number of cases, the heterogeneous group of patients and types of procedures performed, as well as the short follow-up period, the comparison between the techniques and the relationship with their outcomes limit the results of our study. Lasty, the accuracy of the results may be affected by retrospective analysis of data.
CONCLUSION
In our study, the hybrid treatment of aortic arch disease proved to be a technically feasible alternative with short and medium term results.
The involvement of the ascending aorta by type A dissection and the need to implant in Zone 0 had a higher rate of acute neurological events and retrograde type A dissection.
The treatment success rates and required reinterventions in the various segments of the aortic arch treated demonstrate the need for rigorous follow-up of these long-term patients.
REFERENCES
1. Moulakakis KG, Mylonas SN, Markatis F, Kotsis T, Kakisis J, Liapis CD. A systematic review and meta-analysis of hybrid aortic arch replacement. Ann Cardiothorac Surg. 2013;2(3):247-60. [MedLine]
2. Ingrund JC, Nasser F, Jesus-Silva SG, Limaco RP, Galastri FL, Burihan MC, et al. Hybrid procedures for complex thoracic aortic diseases. Rev Bras Cir Cardiovasc. 2010;25(3):303-10. [MedLine] View article
3. De Rango P, Cao P, Ferrer C, Simonte G, Coscarella C, Cieri E, et al. Aortic arch debranching and thoracic endovascular repair. J Vasc Surg. 2014;59(1):107-14. [MedLine]
4. Czerny M, Weigang E, Sodeck G, Schmidli J, Antona C, Gelpi G, et al. Targeting landing zone 0 by total arch rerouting and TEVAR: midterm results of a transcontinental registry. Ann Thorac Surg. 2012;94(1):84-9. [MedLine]
5. Cao P, De Rango P, Czerny M, Evangelista A, Fattori R, Nienaber C, et al. Systematic review of clinical outcomes in hybrid procedures for aortic arch dissections and other arch diseases. J Thorac Cardiovasc Surg. 2012;144(6):1286-300.
6. Vallejo N, Rodriguez-Lopez JA, Heidari P, Wheatley G, Caparrelli D, Ramaiah V, et al. Hybrid repair of thoracic aortic lesions for zone 0 and 1 in high-risk patients. J Vasc Surg. 2012;55(2):318-25. [MedLine]
7. Andersen ND, Williams JB, Hanna JM, Shah AA, McCann RL, Hughes GC. Results with an algorithmic approach to hybrid repair of the aortic arch. J Vasc Surg. 2013;57(3):655-67.
8. Bavaria J, Vallabhajosyula P, Moeller P, Szeto W, Desai N, Pochettino A. Hybrid approaches in the treatment of aortic arch aneurysms: postoperative and midterm outcomes. J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S85-90. [MedLine]
9. Benedetto U, Melina G, Angeloni E, Codispoti M, Sinatra R. Current results of open total arch replacement versus hybrid thoracic endovascular aortic repair for aortic arch aneurysm: a meta-analysis of comparative studies. J Thorac Cardiovasc Surg. 2013;145(1):305-6. [MedLine]
10. Mitchell RS, Ishimaru S, Ehrlich MP, Iwase T, Lauterjung L, Shimono T, et al. First International Summit on Thoracic Aortic Endografting: roundtable on thoracic aortic dissection as an indication for endografting. J Endovasc Ther. 2002;9(Suppl 2):II98-105. [MedLine]
11. Shirakawa Y, Kuratani T, Shimamura K, Torikai K, Sakamoto T, Shijo T, et al. The efficacy and short-term results of hybrid thoracic endovascular repair into the ascending aorta for aortic arch pathologies. Eur J Cardiothorac Surg. 2014;45(2):298-304. [MedLine]
12. Novero ER, Metzger PB, Obregon J, Marco VLA, Rossi FH, Moreira SM. Endovascular treatment of thoracic aortic diseases: a single center result analysis. Radiol Bras. 2012;45(5):251-8.
13. Metzger PB, Fontes DCC, Novero ER, Marco VLA, Moreira SM, Rossi FH, et al. Tratamento endovascular da dissecção crônica de aorta tipo B complicada. Rev Bras Cardiol Invasiva. 2012;20(2):184-90.
14. Cho JS, Haider SE, Makaroun MS. US multicenter trials of endoprostheses for the endovascular treatment of descending thoracic aneurysms. J Vasc Surg. 2006;43(Suppl A):12A-9A.
15. Patel HJ, Nguyen C, Diener AC, Passow MC, Salata D, Deeb GM. Open arch reconstruction in the endovascular era: analysis of 721 patients over 17 years. J Thorac Cardiovasc Surg. 2011;141(6):1417-23. [MedLine]
16. Iba Y, Minatoya K, Matsuda H, Sasaki H, Tanaka H, Kobayashi J, et al. Contemporary open aortic arch repair with selective cerebral perfusion in the era of endovascular aortic repair. J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S72-7. [MedLine]
17. Sachs T, Pomposelli F, Hagberg R, Hamdan A, Wyers M, Giles K, et al. Open and endovascular repair of type B aortic dissection in the Nationwide Inpatient Sample. J Vasc Surg. 2010;52(4):860-6.
18. Cowan JA Jr, Dimick JB, Henke PK, Huber TS, Stanley JC, Upchurch GR Jr. Surgical treatment of intact thoracoabdominal aortic aneurysms in the United States: hospital and surgeon volume-related outcomes. J Vasc Surg. 2003;37(6):1169-74. [MedLine]
19. Patel VI, Mukhopadhyay S, Ergul E, Aranson N, Conrad MF, Lamuraglia GM, et al. Impact of hospital volume and type on outcomes of open and endovascular repair of descending thoracic aneurysms in the United States Medicare population. J Vasc Surg. 2013;58(2):346-54. [MedLine]
20. Chikwe J, Cavallaro P, Itagaki S, Seigerman M, Diluozzo G, Adams DH. National outcomes in acute aortic dissection: influence of surgeon and institutional volume on operative mortality. Ann Thorac Surg. 2013;95(5):1563-9. [MedLine]
21. Lotfi S, Clough RE, Ali T, Salter R, Young CP, Bell R, et al. Hybrid repair of complex thoracic aortic arch pathology: long-term outcomes of extra-anatomic bypass grafting of the supra-aortic trunk. Cardiovasc Intervent Radiol. 2013;36(1):46-55. [MedLine]
22. Metzger PB, Novero ER, Rossi FH, et al. Evaluation of preoperative computed tomography angiography in association with conventional angiography versus computed tomography angiography only, in the endovascular treatment of aortic diseases. Radiol Bras. 2013;46(5):265-72.
23. Fioranelli A, Razuk Filho A, Castelli Júnior V, Karakhanian W, Godoy JM, Caffaro RA. Mortality within the endovascular treatment in Stanford type B aortic dissections. Rev Bras Cir Cardiovasc. 2011;26(2):250-7. [MedLine] View article
24. Schoder M, Lammer J, Czerny M. Endovascular aortic arch repair: hopes and certainties. Eur J Vasc Endovasc Surg. 2009;38(3):255-61. [MedLine]
25. Gehringhoff B, Torsello G, Pitoulias GA, Austermann M, Donas KP. Use of chimney grafts in aortic arch pathologies involving the supra-aortic branches. J Endovasc Ther. 2011;18(5):650-5. [MedLine]
No financial support.
Authors' roles & responsibilities
PBM: Analysis and/or interpretation of data, statistical analysis, final approval of the manuscript, conception and design of the study, operations and/or experiments, manuscript writing or critical review of its contents
FHR: Final approval of the manuscript, operations and/or experiments, manuscript writing or critical review of its contents
SMM: Final approval of the manuscript, operations and/or experiments
MI: Final approval of the manuscript, operations and/or experiments
NMI: Final approval of the manuscript, operations and/or experiments
JJD: Final approval of the manuscript, operations and/or experiments
DSN: Operations and/or experiments
AMK: Final approval of the manuscript, operations and/or experiments, manuscript writing or critical review of its contents
Article receive on Monday, January 27, 2014
 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license