ABSTRACT
Objectives: To evaluate the effect of BMI (body mass index) in the postoperative period of elderly patients undergoing CABG.
Methods: Cross-sectional retrospective study, carried out in academic hospital, with all patients (n=290), aged or above 60 years, undergone CABG, from August 2006 to July 2007. The patients were divided into tertiles of BMI (<22, 22-27,> 27kg/m²). The variables included in the study were collected from medical records of patients and analyzed by logistic regression in association with the categories of BMI.
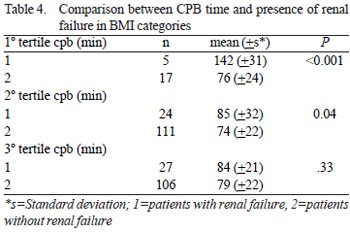
Results: In the group with malnutrition were found larger percentage of impaired lung, kidney, hospital stay and immediate surgical mortality; but without statistical significance. Among female patients, the group malnutrition and eutrophy, 61.5% had hospital stay for a period longer than seven postoperative days compared to 42.5% male patients (P=0.003). In the group with malnutrition was found association between the CPB time and renal dysfunction with P<0.001 and, in eutrophic group with P=0.04. Obesity obtained protective association for lung dysfunction (RR=0.99), readmissions (RR=0.45) and mortality (RR = 0.77), and risk factor for renal dysfunction (RR=1.12).
Conclusions: In short-term, elderly with lower BMI may have increased the risk for complications. In contrast, obesity can have a protective effect, except for renal dysfunction.
RESUMO
Objetivo: Avaliar o efeito do índice de massa corporal (IMC) no pós-operatório de pacientes idosos submetidos a cirurgia de revascularização do miocárdio (CRM).
Métodos: Estudo transversal e retrospectivo, realizado em hospital acadêmico, com todos os pacientes (n=290), com idade igual ou superior a 60 anos, submetidos a CRM, no período de agosto de 2006 a julho de 2007. Os pacientes foram divididos em tercis de IMC (<22, 22-27, >27 kg/m²). As variáveis incluídas no estudo foram coletadas a partir dos prontuários dos pacientes e analisadas por meio de regressão logística na associação com as categorias de IMC.
Resultados: No grupo com magreza foram encontrados maiores percentuais de disfunção pulmonar, renal, permanência hospitalar e mortalidade cirúrgica imediata; porém sem significância estatística. Dos pacientes do sexo feminino, do grupo magreza e eutrofia, 61,5% tiveram permanência hospitalar por um período maior que sete dias pós-operatório; contra 42,5% do sexo masculino (P=0,003). No grupo com magreza, foi encontrada associação entre o tempo de circulação extracorpórea (CEC) e a disfunção renal com P < 0,001 e, no grupo eutrófico com P=0,04. A obesidade obteve associação protetora para disfunção pulmonar (RR=0,99), reinternações (RR=0,45) e mortalidade (RR=0,77), e fator de risco para disfunção renal (RR=1,12).
Conclusões: Em curto prazo, idosos com menor IMC podem ter o risco para complicações aumentado. Em contraste, a obesidade pode exercer um efeito protetor, com exceção da disfunção renal.
INTRODUCTION
The aging process of the population is associated with the increased prevalence of chronic degenerative diseases, especially cardiovascular diseases [1,2]. Thus, it is estimated that an increasing number of senior citizens (60 years of age or older), will undergo CABG [3], although the complications and the risk factors of CABG in that age group are not yet well-established.
Preoperative evaluation of cardiovascular risk includes clinical markers, functional capacity and the specific risk of surgery. Elderly patient present changes in morphology and vascular function [4], increasing the incidence of mortality surrounding the date of surgery, as well as complications such as renal failure, prolonged ventilation, stroke, and postoperative cardiac arrest [5].
The nutritional habits of elderly patients is part of the preoperative evaluation, and there is no gold standard for the diagnosis of nutritional disorders [6], which reveals the need for research. The World Health Organization (WHO) [7] recognized Body Mass Index (BMI), or the Quetelet Index, as the international standard [8]; this parameter uses the patient's weight and height as diagnostic criteria:
BMI = weight (kg)/height (m)².
BMI is used in most epidemiological studies as an indicator of nutritional habits due to its ease of use and its correlation with morbidity and mortality [9]. The effect of BMI on morbidity and mortality differs between young adults and the elderly. Stevens et al. [10] found that the relative risk of death associated with excess weight is lower for older patients.
It is known that patients with cardiac cachexia or obesity can not tolerate heart surgery very well [11,12]. However, the relationship between BMI and its effect on postoperative CABG is controversial: some studies found no significance between high BMI and mortality [13-16]; others have shown a positive correlation between obesity and postoperative complications [17-19]. Gurm et al. [20] found a short-term protective effect of obesity in patients who had undergone CABG.
This study aims to retrospectively evaluate the effect of BMI in the immediate postoperative period of elderly patients who have undergone CABG.
METHODS
A retrospective cross-section study was performed with all patients (n=290), 60 years or older undergoing CABG in the IC/FUC (Institute of Cardiology/ University Cardiology Foundation - Rio Grande do Sul, Brazil) from August 2006 to July 2007. The World Health Organization (WHO) [21] suggests 60 years or older as the definition of the elderly population in developing countries.
Elderly patients under procedures associated with CABG, such as valve replacement or valve repair, transplantation, and pacemaker implants, were excluded from the study, as were those who did not present the protocols completed correctly and those who underwent the procedure without cardiopulmonary bypass.
Data collection
The variables included in the study were collected from patients' medical records. The identification data, co-morbidities and preoperative exams were retrieved from the protocol of preoperative assessment, the transoperative variables were retrieved from the assessment surgical protocol, and the postoperative variables were retrieved from hospital discharge record. All protocols were filled by responsible medical teams and are described below:
Data identifying age, gender, weight, height; Comorbidities: systemic arterial hypertension, prior acute myocardial infarction, heart failure, type 2 Diabetes Mellitus, chronic renal failure, chronic obstructive pulmonary disease, smoking; Preoperative laboratory tests: hematocrit, hemoglobin, creatinine, fasting plasma glucose; Transoperative variables: time of cardiopulmonary bypass (CPB), time of aortic clamping; Postoperative variables: respiratory and renal complications, hospital stay, readmissions and immediate surgical mortality.
Postoperative Complications
Respiratory complications were defined as the inability to remove the patient from artificial respiration in a period exceeding 24 hours, the presence of SARS (Severe Acute Respiratory Syndrome), pulmonary embolism, or severe and persistent atelectasis.
Slight renal failure was defined as creatinine levels increased to 1.3 mg/dl, and mild to severe renal failure was defined as creatinine levels increased to 2.0 mg/dl, and/or with the use of dialysis.
Lengthy hospital stay was defined as one over seven postoperative days, according to the institution's protocol. Re-hospitalizations was defined as those that occurred within the first 30 postoperative days, and deaths were considered immediate surgical mortality if they occurred within the first 30 postoperative days in the hospital.
Determination of Body Mass Index (BMI)
BMI was obtained by dividing body weight (in kilograms) by height (in meters squared) (kg/m²). BMI classification followed the standards established for the elderly according Lipschitz (22) and was divided into tertiles respectively: BMI <22Kg/m² thinness - malnutrition (1
st tertile), 22kg/m²
nd tertile) and BMI>27Kg/m² overweight (3rd tertile).
Statistical analysis
Statistical analysis was performed with SPSS 15.0 software. The variables were assessed descriptively in relation to their frequency, mean and standard deviation. We used the Student t test for continuous variables, and chi-square test for categorical variables. Significance level was set at 5%. The magnitude of the effect was estimated using the relative risk.
This study was reviewed and approved by the Research Ethics Committee of the Institute of Cardiology / University Cardiology Foundation - Rio Grande do Sul, Brazil.
RESULTS
Patient Profiles
The mean age (± standard deviation) of the 290 patients was 68 years (+ 6 years). 65.2% were male. The correlation between BMI and age at surgery was negative (r= -0.1). Regarding the multivariate analysis of gender due to comorbidities, only smoking was statistically significant, with a P <0.001 for males, regardless of BMI.
Table 1 describes the preoperative profile of the patients organized by BMI category. The patients in the 1st tertile (BMI <22kg/m² - thinness) presented higher rates of prior myocardial infarction (36.6%), chronic renal failure (4.5%), chronic obstructive pulmonary disease (18.8%) and smoking (63.6%).
The mean of preoperative laboratory tests and the transoperative variables are described in Table 2. There was significant difference between the categories of BMI only in relation to the longer time of CPB for the patients from the 1st tertile (mean 91 min + 37 min, P=0.01).
Postoperative complications
The prevalence of pulmonary dysfunction, renal failure, re-admissions, extended hospital stays and immediate surgical mortalities in the different BMI categories are described in Figure 1 and Table 3. Chronic renal failure and hospital stays of more than seven postoperative days were the most common complications. In the group of patients of the 1st tertile, higher rates of pulmonary dysfunction, renal failure, extended hospital stay and immediate surgical mortality were found, but without statistical significance.

Fig. 1 - Prevalence of Postoperative Complications by BMI Category; BMI- Body Mass Index

The mean time of hospital stay for all patients as a single group - with or without complications - was 9.47 days with a standard deviation of 9.20 days. Among female patients, the 1st and 2nd tertiles, 61.5% had a hospital stay for a period longer than seven postoperative days, compared to 42.5% of male patients (P=0.003).
The relative risk of poor clinical outcomes related to the patients of the 3rd tertile (BMI> 27kg/m² obesity) showed protective association of obesity to pulmonary dysfunction (RR = 0.99, 95% CI = 0.52 - 0.83), re-admission (RR = 0.45, 95% CI = 0.18 - 1.13) and mortality (RR = 0.77, 95% CI = 0.26 - 2.24), and a risk factor for renal failure (RR = 0.45, 95% CI = 0.18 - 1.13).
In the group of patients in the 1st tertile (Table 4), a correlation was found between the time of CPB and renal failure, with P<0.001 (for renal dysfunction with CPB = 142 min. + 31 min versus renal failure without CPB = 76min + 24min), and, in the 2nd tertile group, with p=0.04 (for renal failure with CPB = 85 min. + 32 min versus without renal failure with CPB = 74 + 22 min).
DISCUSSION
The results of this study showed that low BMI (patients of the 1st tertile) may increase the frequency of postoperative complications in elderly patients undergoing coronary artery bypass grafting. Although the findings do not have statistical significance, it is known that malnutrition in the elderly is associated with increased mortality, as well as susceptibility to infections and reduced quality of life [23]. Malnourishment can impair an elderly patient's ability to manage stress, especially if they are suffering from organ complications or other serious diseases, which results in a higher rate of postoperative complications [24-25].
In malnourished and eutrophic patients, we found a positive correlation between CPB time and renal failure caused by increased creatinine levels, but we also found an association with immediate surgical mortality. Glomerular function declines with age, but studies show that renal failure during heart surgery is a frequent complication; noted more often when CPB time exceeds 90 minutes, confirming the findings of the sample [26-28].
A risk for renal failure was also attributed to obese patients, but without statistical significance. In a recent publication on the relationship between excess weight and risk for chronic renal failure showed that the risk of renal failure is three times higher for obese patients [29]. This finding supports the importance of the relationship of obesity to postoperative renal failure found in the sample studied.
Data analysis showed a benefit in survival of euthrophic and overweight patients; similar to findings published by Brikmeyer et al. [17], Gurm et al. [18] and Fasol et al. [30], in which a BMI superior to 30 kg/m² was not associated with increased mortality [31].
The increased time of hospital stay in this age group is reported in the literature when compared to surgery in younger patients [32,33]. Women from malnutrition and eutrophy groups had longer hospital stays. According to the literature [34] this disparity is because women are at an increased risk for complications and mortality in heart surgery, independent of BMI. Women have arteries of smaller diameters; there is a tendency for women to receive diagnosis and treatment in more advanced phases; and hormonal factors, such as the decrease in estrogen, may interfere with the risk analysis between the genders.
There are limitations to this study. BMI is used in most epidemiological studies, has good correlation with body weight (r=0.80), low correlation with height, but it does not express the quantity or the distribution of body fat [35,36]. In the elderly, there is controversy about the cut-off points. It is believed that the aforementioned values adopted for young adults are most appropriate to prevent malnutrition [22]. The aging process is followed by a decrease in height, an accumulation of fat tissue and lean body mass reduction, which limits the use of BMI [37]. Another limitation is the type and location of body fat, because there are differences in risk of cardiovascular disease among patients in the android standard (accumulation of visceral fat with central or abdominal distribution) compared to standard gynecoid (accumulation of gluteal-femoral fat).
CONCLUSION
BMI can have an effect on the complications of coronary artery bypass grafting in elderly; lower BMI may increase the risk for complications. In contrast, obesity may have a protective effect, but this effect is not found in cases of renal failure. This study focused only on short-term data. Long-term conclusions need further investigation.
REFERENCES
1. Truelsen T, Bonita R, Jamrozik K. Survillance of stroke: a global perspective. Int J Epidemiol. 2001;30(Suppl 1):S11-6. [MedLine]
2. Kilsztajn S, Rossbach A, Câmara MB, Carmo MSN. Serviços de Saúde, gastos e envelhecimento da população brasileira. Rev Bras Estud Popul. 2003;20(1):93-108.
3. Jaeger AA, Hlatky MA, Paul SM, Gortner SR. Functional capacity after cardiac surgery in elderly patients. J Am Coll Cardiol. 1994;24(1):104-8. [MedLine]
4. Priebe HJ. The aged cardiovascular risk patient. Br J Anaesth. 2000;85(5):763-78. [MedLine]
5. Lakatta EG. Cardiovascular aging in health. Clin Geriatr Med. 2000;16(3):419-44. [MedLine]
6. Acuña K, Cruz T. Avaliação do estado nutricional de adultos e idosos e situação nutricional da população brasileira. Arq Bras Endocrinol Metab. 2004;48(3):345-61.
7. WHO, World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. Geneva:World Health Organization;1998.
8. Willett W. Nutritional epidemiology. 2nd ed. Oxford:Oxford University Press;1998.
9. Anjos LA. Índice de massa corporal (massa corporal x estatura2) como indicador do estado nutricional de adultos: revisão da literatura. Rev Saúde Pública. 1992;26:431-6.
10. Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338(1):1-7. [MedLine]
11. Engelman DT, Adams DH, Byrne JG, Aranki SF, Collins JJ Jr, Couper GS, et al. Impact of body mass index and albumin on morbidity and mortality after cardiac surgery. J Thorac Cardiovasc Surg. 1999;118(5):866-73. [MedLine]
12. Rapp-Kesek D, Ståhle E, Karlsson TT. Body mass index and albumin in the preoperative evalution of cardiac surgery patients. Clin Nutr. 2004;23(6):1398-404. [MedLine]
13. Rockx MA, Fox SA, Stitt LW, Lehnhardt KR, McKenzie FN, Quantz MA, et al. Is obesity a predictor of mortality, morbidity and readmission after cardiac surgery? Can J Surg. 2004;47(1):34-8. [MedLine]
14. Cheung W. Outcomes of the morbidly obese having cardiac surgery. Crit Care Resusc. 2005;7(3):172. [MedLine]
15. Maurer MS, Luchsinger JA, Wellner R, Kukuy E, Edwards NM. The effect of body mass index on complications from cardiac surgery in the oldest old. J Am Geriatr Soc. 2002;50(6):988-94. [MedLine]
16. Yap C, Zimmet A, Mohajeri M, Yii M. Effect of obesity on early morbidity and mortality following cardiac surgery. Heart Lung Circ. 2007;16(1):31-6. [MedLine]
17. Wigfield CH, Lindsey JD, Muñoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI > or = 40. Eur J Cardiothorac Surg. 2006;29(4):434-40. [MedLine]
18. Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Obesity and risk of new-onset atrial fibrillation after cardiac surgery. Circulation. 2005;112(21):3247-55. [MedLine]
19. Birkmeyer NJ, Charlesworth DC, Hernandez F, Leavitt BJ, Marrin CA, Morton JR, et al. Obesity and risk of adverse outcomes associated with coronary artery bypass surgery. Northern New England Cardiovascular Disease Study Group. Circulation. 1998;97(17):1689-94. [MedLine]
20. Gurm HS, Whitlow PL, Kip KE; BARI Investigators. The impact of body mass index on short- and long-term outcomes inpatients undergoing coronary revascularization. Insights from the bypass angioplasty revascularization investigation (BARI). J Am Coll Cardiol. 2002;39(5):834-40. [MedLine]
21. WHO, World Health Organization. Population ageing: a public health challenge. Geneva:World Health Organization;1998. Fact Sheet n.135.
22. Lipschitz DA. Screening for nutritional status in the elderly. Prim Care. 1994;21(1):55-67. [MedLine]
23. Perissinotto E, Pisent C, Sergi G, Grigoletto F; ILSAWorking Group (Italian Longitudinal Study on Ageing). Anthropometric measurements in the elderly: age and gender differences. Br J Nutr. 2002;87(2):177-86. [MedLine]
24. Landi F, Zuccalà G, Gambassi G, Incalzi RA, Manigrasso L, Pagano F, et al. Body mass index and mortality among older people living in the community. J Am Geriatr Soc. 1999;47(9):1072-6. [MedLine]
25. Lesourd B. Immune response during disease and recovery in the elderly. Proc Nutr Soc. 1999;58(1):85-98. [MedLine]
26. Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15(6):816-23.
27. Taniguchi F, Souza A, Martins AS. Tempo de circulação extracorpórea como fator de risco para insuficiência renal aguda. Rev Bras Cir Cardiovasc. 2007;22(2):201-5. [MedLine]
28. Sear JW. Kidney dysfunction in the postoperative period. Br J Anaesth. 2005;95(1):20-32. [MedLine]
29. Bedogni G, Pietrobelli A, Heymsfield SB, Borghi A, Manzieri AM, Morini P, et al. Is body mass index a measure of adiposity in elderly women? Obes Res. 2001;9(1):17-20. [MedLine]
30. Fasol R, Schindler M, Schumacher B, Schlaudraff K, Hannes W, Seitelberger R, et al. The influence of obesity on perioperative morbidity: retrospective study of 502 aortocoronary bypass operations. J Thorac Cardiovasc Surg. 1992;40(3):126-9.
31. Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study. Int J Obes Relat Metab Disord. 2001;25(11):1730-5. [MedLine]
32. Salomon NW, Page US, Bigelow JC, Krause AH, Okies JE, Metzdorff MT. Coronary artery bypass grafting in elderly patients. Comparative results in a consecutive series of 469 patients older than 75 years. J Thorac Cardiovasc Surg. 1991;101(2):209-17.
33. Gersh BJ, Kronmal RA, Schaff HV, Frye RL, Ryan TJ, Mock MB, et al. Comparison of coronary artery bypass surgery and medical therapy in patients 65 years of age or older. A nonrandomized study from the Coronary Artery Surgery Study (CASS) registry. N Eng J Med. 1985;313(4):217-24.
34. Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144(1):21-8. [MedLine]
35. Cervi A, Franceschini SC, Priore SE. Análise crítica do uso do índice de massa corporal para idosos. Rev Nutr 2005;18(6):765-75.
36. Santos DM, Schieri R. Índice de massa corporal e indicadores antropométricos de adiposidade em idosos. Rev Saúde Pública. 2005;39(2):163-8.
37. Beliveau MM, Multach M. Perioperative care for the elderly patient. Med Clin North Am. 2003;87(1):273-89. [MedLine]
1. MD Student in Medical Sciences - UFRGS (Specialist in Cardiology Nutrition - ICFUC-RS)
2. MD in Health Sciences (Cardiology) ICFUC-RS (Professor of the Professional School of the University Cardiology Foundation; Coordinator of Health Multiprofessional Residency (Nutrition) of the ICFUC-RS).
3. Graduate Student in Nutrition UNISINOS (Nutritionist)
This study was carried out at IC/FUC (Institute of Cardiology/ University Cardiology Foundation - Rio Grande do Sul)
Correspondence address:
Cíntia Reis
R. São Manoel - 229/1 - Rio Branco
Porto Alegre - RS. CEP 90620-110
E-mail: nutri.cissa@yahoo.com.br
Article received on March 18th, 2008
Article accepted on September 23rd, 2008
Article receive on Tuesday, March 18, 2008




 All scientific articles published at rbccv.org.br are licensed under a Creative Commons license
All scientific articles published at rbccv.org.br are licensed under a Creative Commons license